

News and analysis of current issues affecting health care providers and payers
the patient experience
Health care reform, the newly insured and a growing interest in population health management have intensified the market’s interest in telehealth technologies and services. In looking to extend capabilities and patient interactions beyond traditional care settings, health care providers are developing integrated strategies for adopting telehealth technologies — as
more payers and employers begin to pay for these services and as the value of these tools is increasingly quantified. A recent study from business information provider IHS predicts the
US telehealth market will grow from $240 million in revenue in 2013 to $1.9 billion in 2018 —
an annual growth rate of more than 50%.
The anticipated surge is due in part to the current physician shortage and an expanded patient base under the Patient Protection and Affordable Care Act. Key also to the move toward telehealth are efforts to put consumers at the center of their own health care — maximizing the power of technology innovations for virtual care, where patients can get the care they need where and when they need it. In this Health Care Industry Post, we look at how the industry is leveraging telehealth technologies, as well as strategic considerations for organizations seeking to launch a sustainable telehealth program.

What is telehealth? Defining the terms
With telehealth technologies, providers can deliver quality care at a lower cost, a critical imperative in the accelerating era of value-based payment. Other key benefits are profiled below.
Increasing access to care and reaching new markets
In enabling virtual consultation regardless of geographic location, telehealth is perceived
as a way to increase patients’ access to care — particularly for those who live in rural and underserved areas. Also, as more seniors and patients with chronic diseases choose to remain at home rather than entering a care facility,
telehealth can be a vital link in cost-effective health care maintenance.
Telehealth can also give providers a competitive advantage by enabling them to reach new markets. Because the digital realm is global, providers leveraging telehealth can connect with patients
in remote areas and global markets. Patients who begin with a virtual exam and diagnostics may develop relationships that could lead to direct care activities.
Reducing emergency room visits and hospitalizations
Telehealth can help improve treatment compliance through daily monitoring and early care team intervention to address problems before they become acute. The Federal Communications Commission reports that remote patient monitoring for such chronic conditions as heart disease, pulmonary disease and diabetes could save $197 billion nationwide over 25 years.
Enabling collaboration and optimizing resources
In the push for care delivery to become more integrated, telehealth offers a prime channel for multiple providers to communicate within a single episode of care, while centralizing all available data, reducing repeated tests and streamlining data collection. It also enables greater use of
scarce clinical resources, bridging the gap between clinician supply and patient demand.
Telehealth is defined as the use of technology
to deliver health care, health information or health education at a distance. Sometimes referred to as telemedicine, e-health or
e-medicine, telehealth is the all-inclusive term for the world of virtual care delivery.
Telehealth communication is used in two settings: between a health care provider and a patient in a different location or between two clinicians where one provider wants to
consult with or have the patient consult with a specialist in another location. Communication can take place 1) synchronously, or in
Advancing patient-centered care
Through remote monitoring, automated follow-ups and readily accessible communication channels, providers are empowered to deliver the support and guidance that many patients need as they
go through the day-to-day healing process. Continuous connection can ensure that patients are following their treatment plans as well as modifying for any needed adjustments.
While other industries have readily transformed their business models with internet, mobile technology and other digital advancements, the health care industry has proceeded carefully. High investment costs and uncertain return on investment have created a tenuous economic model for digital expansion. The health care industry also faces other unique obstacles, profiled below.
Navigating reimbursement challenges
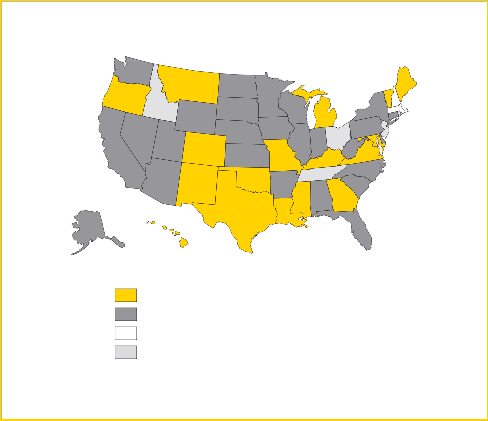
Limited reimbursement continues to be a
major barrier to telehealth expansion, although telehealth payment policies are evolving nationally (see Exhibit 1) and state by state (see Exhibit 2).
A recent study (“Telehealth among US hospitals,”
Health Affairs, February 5, 2014) finds that 42%
“real time,” through video conferencing or
2) asynchronously, or “anytime,” through store-and-forward technology that transmits digital information for later response.
Real-time telehealth can closely resemble a typical clinic visit, the difference being that patient and physician are not in the
same location. Store-and-forward telehealth is typically used for monitoring patients remotely and managing chronic disease, where patient and physician, or physician and physician, do not require face-to-
face communication.
of US hospitals have telehealth capabilities, noting that state policies requiring reimbursement at
the same rate as face-to-face services increase the likelihood that providers will adopt telehealth programs. Teaching hospitals, those equipped with additional advanced medical technology, larger health care systems and nonprofit organizations are more likely to offer telehealth services.
Medicare
Medicare pays for some telehealth services, especially in remote rural areas, but has several restrictions. The patient must be located in an eligible location and in an eligible facility, and
must be seen by an eligible provider for an eligible Current Procedure Terminology (CPT®) billing code. Medicare reimburses the facility a small “facility fee” that is adjusted regularly. A significant portion of telehealth services are store-and-forward rather than real-time, but Medicare generally covers only real-time services.
Medicaid
According to the National Conference of State Legislatures (NCSL), the most common route states are taking is to cover telehealth services in the Medicaid program. To date, 43 states and the
District of Columbia provide some form of Medicaid reimbursement for telehealth services.
Private payers
As with Medicaid, regulations for telehealth reimbursement by private payers are set by the
2 Health Care Industry Post News and analysis of current issues affecting health care providers and payers
“We must ensure that our regulatory environment appropriately balances the exciting advances in technology for patients, while still maintaining safeguards that allow innovation. To put it in perspective, the legal structure around telehealth was
established in 2000, when cell phones were still just phones.”
— Former US Senator Tom Daschle
states. The NCSL reports that 19 states and the District of Columbia now require private insurance plans in the state to cover telehealth services. Arizona will join this list in January 2015.
Nontraditional payers for telehealth services range from charitable organizations, long-term care and community health providers to self-insured groups and agencies serving special popuations.
Complying with multiple state laws Differing state policies raise the challenge of violating state licensing and prescribing laws. A
physician who sees a patient through telehealth
in another state must then comply with the local laws in the state where the patient is located.
With 50 different states and sets of laws, multiple compliance factors must be considered. Physicians need to check the current and pending legislation in the states in which they practice.
Ensuring privacy and security
As telehealth services are offered, more sensitive patient data is held and transmitted electronically — opening the door to potential privacy and security breaches. Federal legislation requires health
care organizations to ensure the security of their data from all “reasonably anticipated threats.” Specifically, the Health Insurance Portability and Accountability Act (HIPAA) Security Rule mandates that organizations put in place safeguards to
ensure the confidentiality, integrity and availability of electronic protected health information.
Health care organizations need to implement telehealth in a way that establishes rigorous security measures for reducing risks of telehealth data breaches — from data transmission that
may be intercepted by third parties to the risk of information technology (IT) support staff or other personnel becoming party to a videoconferencing session. Also, data temporarily stored on telehealth devices such as digital diagnostic tools needs to be protected adequately from potential security breaches.
Exhibit 1. Recent telehealth developments at the national and state levels
• The Telehealth Modernization Act, HR 3750, seeks to establish a federal standard for telehealth and clear up the confusion from myriad state policies.
• The TELEhealth for MEDicare (TELE-MED) Act of 2013, HR 3077, would allow Medicare
providers to treat patients electronically across state lines without having to obtain multiple state medical licenses.
• The 21st Century Care for Military & Veterans Act, HR 3507, would expand access to telehealth services for veterans and their families.
• The Centers for Medicare & Medicaid Services announced changes to Medicare’s 2014 physician fee schedule to expand coverage incrementally for telehealth services.
• The Alliance for Connected Care was launched recently by former US Senators Tom Daschle, Trent Lott and John Breaux. The group will focus on raising awareness about the benefits of telehealth, while at the same time pushing for regulations that will not impede patient access to care.
Exhibit 2. States with coverage for telehealth services
Medicaid and private insurance coverage for telehealth
Medicaid coverage for telehealth
Private insurance coverage for telehealth
No required coverage for telehealth/no data
Source: National Conference of State Legislatures, 2014.
3
Surveying the telehealth landscape
Health care organizations are incorporating telehealth technologies to manage costs, broaden access and improve patient care. Here are a few examples of how the technology is being used today:
• WellPoint offers employer and individual plans remote consultations with physicians using laptop webcams and video-enabled smartphones and tablets. Its LiveHealth Online program is included in employer plans in California and Ohio and will be expanded to commercial plans by
late 2014.
• UnitedHealth offers NowClinic telehealth consultations in
22 states.
• Blue Cross Blue Shield’s Online Care Anywhere is currently available to residents in 30 states.
• Humana has launched a year-long pilot program to measure the effects of its “Healthsense eNeighbor”
in-home monitoring technologies on improving health outcomes and reducing readmissions.
• A growing number of large businesses, such as Home Depot, Booz & Co. and Westinghouse Electric, are offering more remote health care consultations in their employee benefit packages.
• Beth Israel Medical Center in New York offers “Teledoc,”
24/7 access to physicians by phone or video consultation.
• Mercy Health Systems in Missouri is building a $90 million Virtual Care Center, the first facility of its kind in the nation. Staffed by hundreds of health care providers, the center will expand Mercy’s telehealth capabilities to outlying care centers across a four-state region.
• In Mississippi, the Diabetes Telehealth Network has launched an 18-month remote care management program, enabling people with diabetes to have more consistent and timely access to clinicians via telehealth technology in their homes.
• The University of California, Berkeley School of Optometry uses telehealth technology to perform retinal scan evaluations for thousands of low-income diabetic patients in a rural part of California.
• A growing number of hospitals are using telehealth systems for local and off-site staff to continually monitor ICU patients’ vital signs. System users report lower ICU staffing requirements, along with reduced length of stay and risk of mortality among ICU patients.
• “Virtual Tumor Boards” — groups of cancer specialists — are using telehealth technology for virtual meetings to review cancer patient treatment options.
• Through telestroke programs around the country — for example, at Mayo Clinic, Dartmouth-Hitchcock and University of Virginia Health System — experts use videoconferencing technology to consult with emergency department staff at community hospitals in diagnosing patients with suspected strokes and conferring on best treatment options.
• A number of health care providers are consulting with patients through Google’s recently launched Helpouts, a video-chat platform that supports HIPAA compliance.
Designing a highly reliable, cost-efficient and sustainable telehealth program begins with understanding the market, including engagement channels and their interrelationships.
Three channels of engagement
A sound telehealth program considers three overlapping and mutually reinforcing channels for market engagement — patients, providers and communities — all of which are enabled
by infrastructure synergies (see Exhibit 3). Synchronous and asynchronous approaches, along with digital communication media, offer technologies that can be applied across channels, establishing stronger market penetration and
economics. Telehealth programs are more likely to succeed when they integrate appropriate services across channels to build multi-faceted relationships with patients, referring physicians and health system partners.
Patients: clinical services
Telehealth technologies, from e-visits to at-a- distance monitoring and consultation, extend the traditional practice of medicine to remote patients — at a cost far below that of visits to
a physician, emergency department or urgent care center. These “virtual house calls” are particularly critical for patients who live in rural and underserved areas.
For patients with chronic diseases, home-based monitoring devices can easily capture and transmit over the internet clinical data such as blood pressure or glucose levels, helping to prevent avoidable hospitalizations and support patient
self-management.
Providers: physician referrals and consultations
For providers, e-consults are enabled by store- and-forward technologies. These technologies electronically transmit prerecorded videos and digital images, such as X-rays, video clips and photos, between primary care providers and medical specialists. Health professionals can consult and collaborate virtually with patients and other clinicians, regardless of geographic location. The result is a cost-effective alternative to physician office visits, increasing provider caseloads without increasing their workloads.
Such remote monitoring services as the e-ICU
provide real-time alerts and notifications that
can significantly improve patient outcomes while reducing resource use, while other services, such
Exhibit 3. Telehealth engagement channels
Patients
Providers Communities
Source: EY, 2014.
as e-trauma, can extend clinical knowledge to remote locations to inform critical decision-making.
Communities: digital communication
For communities, telehealth leverages pervasive technologies to enable cost-effective, timely communications among patients and providers. These may include patient portals to provide advice and answer questions, internet-based clinical content delivered to patients through emails and links to support patient education, or social media to offer lifestyle guidance tailored to disease management groups.
The point of intersection: infrastructure synergies
All channels are fueled by infrastructure synergies that provide connectivity with electronic health records (EHRs) and enable communications
among care facilities, referring physicians and patients. They also provide the link to population- based management databases and other health care analytic functions to measure value in the form of the “Triple Aim” metrics: better care for individuals, better health for populations and lower costs for health care overall.
development, all designed to lead to a scalable,
financially viable enterprise solution.
Clinical services
Infrastructure synergies
Digital communication
Physician referrals and consultation
1. Know your market
Scan external trends to understand telehealth growth opportunities, economic return and execution risk. Consider:
• Macro trends. Assess market size, competitors and their value propositions, as well as reimbursement and other industry trends that impact telehealth delivery.
• Technology trends. Analyze the range of telehealth solutions and supporting technologies available in the market, including their requirements, potential for integration with current systems, and security parameters.
• Customer trends. Capture the stratification of patient and clinician needs and telehealth opportunities along traditional lines — demographic, disease and geographic — from the perspectives of patients, providers
and payers.
• Channel analysis. Explore go-to-market and access channel differences by comparing
the alignment of care delivery and financing stakeholders. Identify win-win perspectives and channels that align value preferences.
2. Set your strategic intent
Define what telehealth success means to your organization, including:
• Community needs. Conduct a needs assessment to identify and prioritize potential telehealth activities that will match gaps in services. Identify how your telehealth program will
provide a solution to current challenges — for example, by reducing avoidable readmissions, helping patients keep their chronic
5
Exhibit 4. Sample metrics for gauging telehealth program success
Source: EY, 2014.
Federal guidelines for mobile health apps
In late September 2013, the U.S. Food and Drug Administration (FDA) issued final guidelines for mobile health apps, outlining the apps that the regulations will affect and the requirements those apps must meet to achieve FDA approval.
The FDA’s approach focuses on regulating apps that carry significant risks if they do not operate correctly — for example, those that enable a physician to make a diagnosis by smartphone or tablet, or that transform a smartphone into an electrocardiography machine to detect abnormal heart rhythms.
The app is considered a device if its intention is to diagnose, treat or prevent disease, or affect the function of the body. Apps that are an extension of medical devices, such as the remote display of data from bedside monitors, are also subject to regulation.
The two categories of apps that will not be regulated are apps that 1) are not medical devices and
2) might meet the definition of a medical device but pose low risk to the public. Apps that will not be regulated include those that help patients:
• Manage their diseases or conditions without providing specific treatment
• Organize and track their health information
• Easily access information on their health conditions or treatments
• Document, show or communicate potential medical conditions to health care providers
Also unregulated are apps for providers that automate simple tasks and enable providers and patients to interact with personal health record or EHR systems.
diseases under control or improving public health statewide.
• Organizational alignment. Assess how your telehealth program aligns with your organization’s overall mission, vision, values and culture.
Assess your capabilities against market opportunities.
3. Design your telehealth program Leveraging the input of a multidisciplinary group of stakeholders, detail all dimensions of your
telehealth program, including:
• Governance. Establish a governance structure, including where clinical and operational oversight resides and who is accountable for telehealth financial performance.
• Revenue model. Define payment type, reimbursement level and value proposition. Determine which services are reimbursable through Medicare, Medicaid and private insurance. Consider other potential funding sources, such as federal or state grants that
fund telehealth programs, foundations that fund innovative projects and vendors, or developers willing to finance telehealth expansion. Create a plan for long-term financial sustainability.
• Human resources. Determine the number
and kinds of staff needed to deliver telehealth services, as well as a plan for staff support, such as physician champions who can promote program benefits to their peers.
• Processes and policies. Develop standardized processes and policies that facilitate high- quality, efficient care, incorporating telehealth as much as possible into current standards to encourage easier adoption.
• Technology. Identify technology solutions to enable telehealth service delivery. Determine the features of telehealth technology that will meet your clinical service needs and business plan. Consider:
• Specialized telehealth technologies for such activities as telemonitoring, remote diagnostics and remote robotics
• General digital solutions that will enhance and facilitate your core connected capabilities, such as mobility solutions, patient portals and call centers
• IT infrastructure needed to support telehealth and digital solutions — consider network
6 Health Care Industry Post News and analysis of current issues affecting health care providers and payers
“In today’s hyper-connected society, the patient and the provider are only a few clicks away. The telephone, cell phone, fax, video, smart devices, and health information technology are not limited by geographic boundaries ... [and] patients expect their trusted providers to be able to treat them anywhere.”
— Reps. Devin Nunes (R-CA) and Frank Pallone (D-NJ) Co-sponsors, TELE-MED Act of 2013
robustness and bandwidth, authentication and authorization capabilities for secure connection, and solutions for integrating telehealth and digital solutions with current systems such as EHRs and billing
Develop technology specifications and invite vendors for demonstrations and performance testing.
• Training. Establish a plan for training, staff licensing and credentialing. Training should span direct users of telehealth technology, such as clinicians and patients, as well as administrators and referring providers.
• Measurement. Determine performance metrics and performance reporting capabilities needed to effectively lead, manage and gauge program success (see Exhibit 4 for sample metrics).
• Parnerships. Identify potential collaborators and partners to alleviate costs, accelerate program implementation and drive innovation, while effectively managing the risk profile
of telehealth growth. Along with vendor partners, consider payers, other providers (for example, hospitals in nearby regions, primary care associations, assisted living
facilities, skilled nursing homes and home care agencies) and nontraditional participants,
such as broad technology, consumer-focused and other companies that are actively
looking at investments in the health care ecosystem. Developing relationships with major employers in your region can also be critical to program success.
4. Implement and improve
Start slowly and roll out the program in phases:
• Map your timeframe. Create an implementation timeline, allowing ample time for securing executive and clinician support; ordering, installing and troubleshooting equipment; training staff; and ensuring required credentialing.
• Test. Test care and technology plans before full launch through a pilot program with a limited number of patients and staff. For example, begin with a teledermatology program in one clinic rather than several specialties in several clinics. Revise protocols and technology as needed before full launch.
• Measure. Quantify return on investment through such gauges as reduced emergency department use, reduced inpatient hospitalizations and readmissions, and expanded services to new
patient populations. Develop tools to evaluate patient and provider satisfaction and to collect data about service users.
• Continuously improve. Integrate changes into your program based on consumer and provider feedback.
As the nation moves from uncoordinated, volume- based delivery of health services to an integrated, patient-centric, value-based model, the industry’s future will hinge on its ability to achieve higher- quality care, improved patient outcomes and
lower costs. In enabling health care organizations to provide “anytime, anywhere” care to patients, operate more efficiently and cost effectively,
and generate new sources of revenue, telehealth programs are an important part of the strategy to achieve these goals.
EY offers a comprehensive set of telehealth capabilities, with a team that includes experienced physicians, nurses, health care executives and IT professionals with e-health and digital experience. For several years, we have been working actively with our clients to understand health care trends — and identify new care delivery approaches and profitable business models at the intersection of patient, provider and community needs.
To learn more, contact:
Bill Fera, Principal, Advisory
Services, Ernst & Young LLP
+1 412 644 0551 or bill.fera@ey.com
7
EY | Assurance | Tax | Transactions | Advisory
About EY
EY is a global leader in assurance, tax, transaction and advisory
services. The insights and quality services we deliver help build trust and confidence in the capital markets and in economies the world over. We develop outstanding leaders who team to deliver on our promises to all
of our stakeholders. In so doing, we play a critical role in building a better working world for our people, for our clients and for our communities.
EY refers to the global organization, and may refer to one or more, of the member firms of Ernst & Young Global Limited, each of which is a separate legal entity. Ernst & Young Global Limited, a UK company limited by guarantee, does not provide services to clients. For more information about our organization, please visit ey.com.
Ernst & Young LLP is a client-serving member firm of
Ernst & Young Global Limited operating in the US.
© 2014 Ernst & Young LLP. All Rights Reserved.
SCORE No. EC0023
1403-1216078 NY ED None
This material has been prepared for general informational purposes only and is not intended to be relied upon as accounting, tax, or other professional advice. Please refer to your advisors for specific advice.
ey.com