CMS broadens reimbursement for remote patient monitoring services
The landscape of US healthcare is changing, both geographically and technologically. Healthcare providers are not only beginning to implement new technologies such as the cloud, artificial intelligence (AI), and the Internet of Things (IoT) into their care modules, but are also shifting care out of the hospital into clinics, and even into patient’s homes. These changes are geared toward making care more patient-centred and cost effective as part of the overall value-based healthcare initiative.
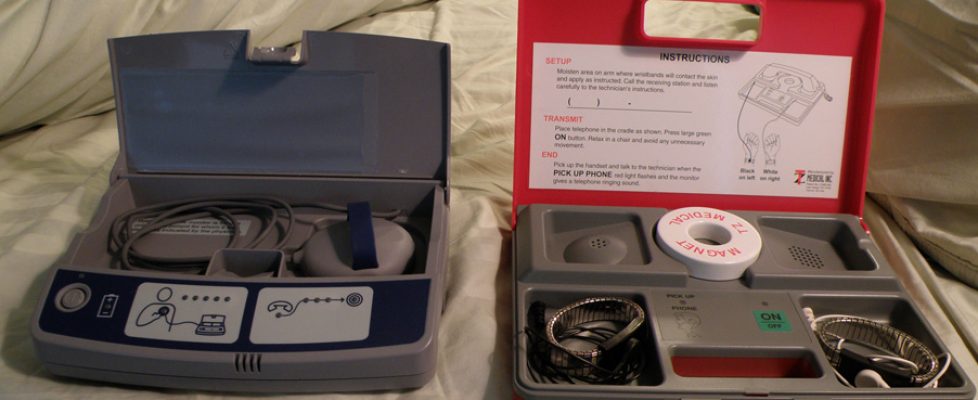
One aspect of moving toward home care is the adoption of telehealth practices; in the US, this adoption is growing, although telehealth still only represents a small portion of the overall healthcare environment. Remote patient monitoring (RPM), a service under the telehealth umbrella, allows the collection of patient medical data in a location that is removed from providers and then safely enables the transfer of the data back to healthcare professionals for evaluation and action. As part of this growing movement to enhance patient access to healthcare, the Centers for Medicare & Medicaid Services (CMS) have released three new Current Procedural Terminology (CPT) codes for the reimbursement of RPM services, which will take effect on January 1, 2019. The three new billing codes—CPT codes 99453, 99454, and 99457—will reimburse physicians for setting up remote monitoring equipment and teaching patients how to use it, for the device’s daily reports or transmissions, and for the time that healthcare staff spend monitoring the data each month, respectively.
The new RPM codes establish a distinct difference from current CMS telehealth reimbursement standards, which are largely built to accommodate rural patients. No such geographic restrictions are placed on the RPM codes, which are available for any patient as long as an in person office visit has occurred in the preceding year. Audio-video interaction between patients and physicians is not required for RPM reimbursement; rather, the coding is set up to facilitate non-face-to-face interaction.
Although its adoption is not currently widespread, the benefits of RPM are expected to help patients avoid unnecessary office visits and reduce overall healthcare costs. RPM can allow physicians to create tailored treatment plans for patients through more informed decisions based on a larger pool of patient-specific data. Outside of the new reimbursement codes, which allow for the monitoring of physiologic parameters, RPM has the potential to track patient adherence to medications or treatment regimens. Such tracking, if used appropriately, would assist physicians in understanding any reasons behind non-compliance and allow for the creation of a personalised plan to improve patient health and avoid more costly medical treatments in the future, particularly for patients with chronic illness. At present, the novel CPT codes aim to incentivise healthcare providers to more effectively incorporate RPM technologies into their practice to efficiently monitor and manage patient needs.