Critical Access Hospitals (CAHs)
Critical Access Hospital is a designation given to eligible rural hospitals by the Centers for Medicare & Medicaid Services (CMS). Congress created the Critical Access Hospital (CAH) designation through the Balanced Budget Act of 1997 (Public Law 105-33) in response to over 400 rural hospital closures during the 1980s and early 1990s. Since its creation, Congress has amended the CAH designation and related program requirements several times through additional legislation.
The CAH designation is designed to reduce the financial vulnerability of rural hospitals and improve access to healthcare by keeping essential services in rural communities. To accomplish this goal, CAHs receive certain benefits, such as cost-based reimbursement for Medicare services. (see What are the benefits of CAH status?)
Eligible hospitals must meet the following conditions to obtain CAH designation:
- Have 25 or fewer acute care inpatient beds
- Be located more than 35 miles from another hospital (exceptions may apply – see What are the location requirements for CAH status?)
- Maintain an annual average length of stay of 96 hours or less for acute care patients
- Provide 24/7 emergency care services
Congress also created the Medicare Rural Hospital Flexibility Program (Flex Program) in the Balanced Budget Act of 1997 to support new and existing CAHs.
This guide provides resources concerning the following CAH-related areas:
- Payment/reimbursement and financial information
- Regulations and information regarding CAH status and the Flex Program
- Key organizations in the field
- Funding opportunities
- Challenges to operation
Frequently Asked Questions
- What are the benefits of CAH status?
- How does Medicaid reimburse CAHs?
- Are all the benefits of CAH status available in every state?
- What types of facilities are eligible for CAH status?
- What are the location requirements for CAH status?
- How many CAHs are there and where are they located?
- What are the quality assurance and quality improvement options for CAHs?
- What is the Medicare Rural Hospital Flexibility Program and how is it related to the CAH program?
- Where can I find CAH comparative information?
- Can a CAH own another healthcare facility?
- Can a CAH add an off-campus, provider-based clinic that does not meet the CAH distance requirements?
- What are the requirements for relocating an existing CAH under the Necessary Provider replacement rules?
- Is there a limit on the length of stay for patients at CAHs?
- How many beds are allowed?
- What is a swing bed?
- What emergency services are CAHs required to provide? What are staffing requirements for emergency services?
- What kinds of agreements does a CAH need to have with an acute care hospital?
- Where can I find examples of CAH network agreements, tools, and other materials?
- How do staffing and other requirements differ for CAHs, compared to general acute care hospitals?
- Are CAHs eligible for the 340B program?
- What sources of capital funding exist for CAHs?
- What is the CAH survey process?
- What legislation has affected the Critical Access Hospital program?
- What are Rural Emergency Hospitals?
- Who can answer questions about CAH status or reimbursement issues?
What are the benefits of CAH status?
CAH status includes the following benefits:
- Cost-based reimbursement from Medicare. As of January 1, 2004, CAHs are eligible for allowable cost plus 1% reimbursement. However, as of April 1, 2013, CAH reimbursement is subject to a 2% reduction due to sequestration. In some states, CAHs may also receive cost-based reimbursement from Medicaid.
- Flexible staffing and services, to the extent permitted under state licensure laws.
- Capital improvement costs included in allowable costs for determining Medicare reimbursement.
- Access to Flex Program educational resources, technical assistance, and/or grants.
For more information about CAH reimbursement and payment benefits, see the Medicare Learning Network: Critical Access Hospital booklet from CMS, the Small Rural Hospital and Clinic Finance 101 manual from the Technical Assistance and Services Center (TASC), or Medicare Payment Basics: Critical Access Hospitals Payment System from the Medicare Payment Advisory Commission (MedPAC).
Critical Access Hospital (CAH) status does not guarantee a better financial situation. Some hospitals will find the cost-based reimbursement advantageous, and some will not. Each hospital must perform its own financial analysis to determine if being a Prospective Payment System (PPS) hospital or a CAH would result in a better financial return. For financially distressed hospitals, even if CAH status leads to increased reimbursement, it may not put the hospital in the black. In fact, some hospitals have closed even after converting to CAH status. The Flex Monitoring Team releases an annual CAH Financial Indicators Report that can be helpful in understanding financial performance of CAHs.
CAH status should be considered or maintained only if it is appropriate for the community need and hospital service area. In particular, consideration should be given to the bed limit for CAHs and potential service lines and whether they are sufficient to meet community need.
CAH status does not necessarily mean fewer services are offered compared to other facilities. Services offered by a CAH should be aimed to meet the community’s unique needs. Therefore, the number and type of services offered in one community may be different than in another community. A CAH can utilize a Community Health Needs Assessment (CHNA) to guide its review of current and future services needs.
For information about payment methods, eligibility criteria, and financial performance, see Medicare Payment for Rural or Geographically Isolated Hospitals and 2016-18 Profitability of Urban and Rural Hospitals by Medicare Payment Classification, which compare the following designations:
- Critical Access Hospital (CAH)
- Sole Community Hospital (SCH)
- Medicare-Dependent Hospital (MDH)
- Rural Referral Center (RRC)
How does Medicaid reimburse CAHs?
Each state determines how it will reimburse CAHs for services through Medicaid. Several states utilize some form of cost-based reimbursement for CAHs, while other states follow a prospective payment system (PPS). Additionally, variation may exist between inpatient and outpatient payment policies.
The Medicaid and CHIP Payment and Access Commission (MACPAC) compiled each state’s Medicaid payment policies for inpatient and outpatient services.
- State Medicaid Payment Policies for Outpatient Hospital Services (July 2016)
State-specific payment details for CAHs are listed in row 28. - State Medicaid Payment Policies for Inpatient Hospital Services (December 2018)
State-specific payment details for CAHs are listed in row 17.
For additional information about your state’s payment policies, consult your State Rural Hospital Flexibility Program Contact.
Are all the benefits of CAH status available in every state?
No. Some states license CAHs under the same licensure rules as other hospitals, and CAHs must comply with those licensure rules. If those rules are stricter than the CAH CoP, the CAH is unable to benefit from the more flexible Medicare Conditions of Participation (CoP) for CAHs and the related cost savings. In addition, five states — Connecticut, Delaware, Maryland, New Jersey, and Rhode Island — do not have any hospitals with CAH status, and therefore do not participate in the Flex Program.
What types of facilities are eligible for CAH status?
Facilities applying to become Critical Access Hospitals must be currently participating in the Medicare program and have a current license as an acute care hospital. Hospitals closed after November 29, 1989, and hospitals that have downsized to health clinic or health center status may also qualify for CAH status if they meet all of the CAH Conditions of Participation.
What are the location requirements for CAH status?
Critical Access Hospitals must be located in rural areas and must meet one of the following criteria:
- Be more than a 35-mile drive from another hospital, or
- Be more than a 15-mile drive from another hospital in an area with mountainous terrain or only secondary roads.
CAHs designated by their state as a Necessary Provider prior to January 1, 2006, are exempt from these distance requirements. See the Centers for Medicare & Medicaid Services’ Clarification of Critical Access Hospital (CAH) Rural Status, Location and Distance Requirements and Critical Access Hospital (CAH) Recertification Checklist for Evaluation of Compliance with the Location and Distance Requirements for definitions.
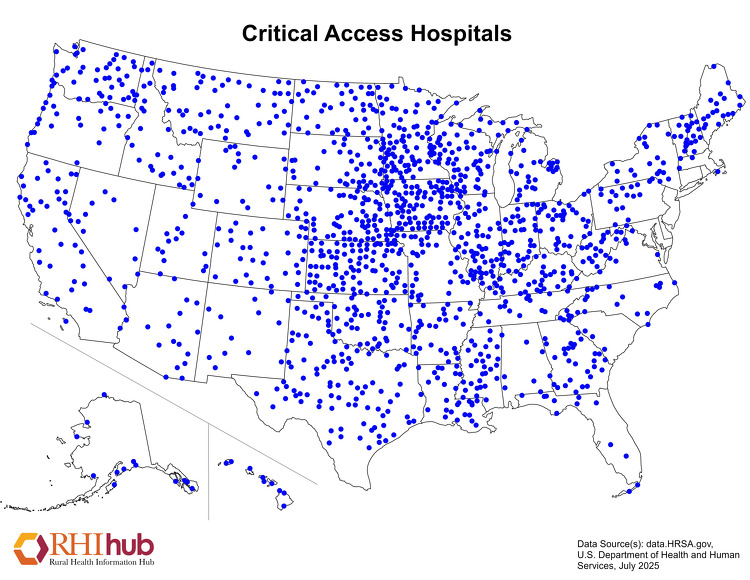
How many CAHs are there and where are they located?
The Flex Monitoring Team maintains a list of Critical Access Hospitals, which includes the hospital name, city, state, zip code, and effective date of CAH status.
As of January 2023, there are 1,358 CAHs located throughout the United States.
The following map shows the locations of Critical Access Hospitals across the United States. State-level healthcare facility maps are also available.
What are the quality assurance and quality improvement options for CAHs?
Critical Access Hospitals (CAHs) must have and maintain quality assurance arrangements with at least one of the following:
- One other CAH or hospital that is part of the network
- One quality improvement organization (QIO) or equivalent entity
- One other appropriate and qualified entity as identified in the state’s rural health care plan, such as an accrediting body.
In addition to quality assurance, quality improvement is important to CAHs. The Medicare Beneficiary Quality Improvement Project (MBQIP), under the Medicare Rural Hospital Flexibility (Flex) Program, aims to improve quality of care in CAHs by encouraging self-reported quality data, which are analyzed and used to inform activities at the facility. The Flex Monitoring Team’s MBQIP Quality Measure Trends, 2011-2016 shows CAH performance trends and MBQIP reporting rates during that period. According to the May 2019 MBQIP Monthly, 99% of CAHs in the U.S. report on at least one domain and 93% reported quality measures in at least three domains in 2018. Any CAH wanting to receive benefits or services from the state’s Flex Program funding must participate in MBQIP and meet the minimum reporting requirements (or submit a waiver if necessary). The National Rural Health Resource Center also provides resources for State Flex Programs and providers regarding MBQIP, including Flex Eligibility Criteria for MBQIP Participation and Waiver Templates.
What is the Medicare Rural Hospital Flexibility Program and how is it related to the CAH program?
The Medicare Rural Hospital Flexibility Program (Flex Program) was created by the Balanced Budget Act of 1997 and is administered through the Federal Office of Rural Health Policy. The Flex Program encourages states to take a holistic approach to strengthening rural healthcare with a focus on Critical Access Hospitals (CAHs) and their Rural Health Clinics, rural emergency medical services (EMS), and rural communities. The Flex Program provides federal cooperative agreements to eligible states to help them achieve their strategic goals, particularly in the following areas for Fiscal Years 2019-2023:
- CAH quality improvement (required)
- CAH operational and financial improvement (required)
- Population health improvement (optional)
- Rural emergency medical services (EMS) improvement (optional)
- Innovative model development (optional)
- Critical Access Hospital designation (required if requested)
Specific goals within each priority area are updated for each program cycle to best reflect the needs of CAHs.
The Federal Office of Rural Health Policy also awarded supplemental funding to eight State Flex Programs to conduct demonstration projects to build an evidence base for rural EMS related to quality metrics and sustainable rural EMS models. Implementation of Flex EMS Supplemental Funding Projects: Year One Activities provides an overview of the implementation of the first year of these efforts, which spanned September 2019 to August 2020.
National infrastructure to support the Flex Program includes:
- Federal Office of Rural Health Policy (FORHP) – Administers the Flex Program and its associated grants to states. Located within the Health Resources and Services Administration (HRSA).
- Technical Assistance and Services Center (TASC) – Provides information and technical assistance to State Flex Programs and Critical Access Hospitals. Located at the National Rural Health Resource Center.
- Flex Monitoring Team – Conducts research and collects data on CAHs, evaluates the impact of the Flex Program, and maintains the list of CAH locations across the country. Also operates and maintains the Critical Access Hospital Measurement and Performance Assessment System (CAHMPAS).
- Rural Quality Improvement Technical Assistance (RQITA) – Seeks to improve healthcare quality and health outcomes in rural communities by providing information and technical assistance to State Flex Programs, Small Health Care Provider Quality Improvement grantees, CAHs, and other rural providers. Located at Stratis Health.
Where can I find CAH comparative information?
The Flex Monitoring Team has a number of resources that would allow you to benchmark your CAH or find data on CAH finances and quality measures. These include:
- The Critical Access Hospital Measurement and Performance Assessment System (CAHMPAS) – Offers the ability to compare data on community-benefit measures at a county and state level and quality indicators at a state level.
- CAH Financial Indicators Report: Summary of Indicator Medians by State – Provides annual state-specific data on revenues, costs, average census, and more. The CAH Financial Indicators Primer and Calculator Resources explains how the measures are calculated and provides tools to enter your own data.
- Patients’ Experiences in CAHs: HCAHPS Results, 2018 – Provides state and national averages for CAH performance on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey and state-specific reports.
- Hospital Compare Quality Measure Results for CAHs, 2018 – Offers state-specific CAH data on inpatient and outpatient quality-reporting measures from Hospital Compare.
- Critical Access Hospital (CAH) State Profiles – Allows users to search for state-level reports on community benefit, quality, and financial indicators by year.
- Community Impact and Benefit Activities of Critical Access, Other Rural, and Urban Hospitals, 2020 – Examines the economic and healthcare benefit of Critical Access Hospitals (CAHs) on rural communities and enables State Flex Programs and CAH administrators to compare the community impact and benefit profiles of CAHs in their state to CAHs and other hospitals nationwide.
The National Rural Health Resource Center’s Population Health Toolkit incorporates County Health Rankings, Hospital Compare, Medicare data, and Census data to help Critical Access Hospitals (CAHs), Flex Coordinators, and rural health networks use a systems-based approach to move towards population health.
If you are interested in comparing the number of beds, operating rooms, or staff, use the HRSA Data Explorer:
- Select “Health Care Facilities” and “Choose Indicators”
- Select indicators of interest, such as “Facility Physicians Full-Time Equivalent,” and “View Data”
- Under “Facility Subcategory,” type in “Critical Access” and select “Contains”
For additional quality reporting information, Medicare’s Care Compare provides data on some CAHs. You can search by state, county, city, or zip code to compare up to three hospitals, or download CMS Provider Data Catalog datasets.
Can a CAH own another healthcare facility?
According to Critical Access Hospital Measurement and Performance Assessment System (CAHMPAS) Data Summary, 60.4% of Critical Access Hospitals managed Rural Health Clinics and 38.4% provided skilled nursing care in 2018.
A survey of Critical Access Hospitals in Illinois found CAHs are most likely to operate (versus own) dental offices, mental health practices, community health centers, retail pharmacies, and EMS, and were most interested in adding community wellness centers and behavioral health practices. The study notes CAHs may choose to collaborate with or operate other facilities rather than owning them, most often citing financial or workforce concerns.
Regarding Federally Qualified Health Centers, see Can another healthcare organization, such as a Critical Access Hospital, own an FQHC? on the Federally Qualified Health Centers topic guide.
Even if a CAH does not own another healthcare facility, it can also benefit from collaboration and network agreements. Demonstrating Critical Access Hospital Value: A Guide to Potential Partnerships identifies potential partners for CAHs and discusses how CAHs can demonstrate their value to them. A Guide for Rural Health Care Collaboration and Coordination, a publication from the Health Resources and Services Administration (HRSA), describes how rural organizations and facilities, including CAHs, can develop partnerships to address the needs of their community.
See Who can answer questions about CAH status or reimbursement issues? for experts to contact for additional guidance on ownership issues.
Can a CAH add an off-campus, provider-based clinic that does not meet the CAH distance requirements?
As of January 1, 2008, all CAHs, including Necessary Provider CAHs that create or acquire an off-campus, provider-based facility, such as a clinic or a psychiatric or rehabilitation distinct part unit, must meet the CAH distance requirement of a 35-mile drive to the nearest hospital or CAH (or 15 miles in the case of mountainous terrain or secondary roads). This provision excludes Rural Health Clinics, as defined under 405.2401(b), from the list of provider-based facilities that must comply with this requirement. Details about this requirement are available in a final rule published in the November 27, 2007 issue of the Federal Register as part of the Medicare Program: Changes to the Hospital Outpatient Prospective Payment System and CY 2008 Payment Rates. See Section XVIII. Changes Affecting Critical Access Hospitals (CAHs) and Hospital Conditions of Participation (CoPs), beginning on page 66877.
What are the requirements for relocating an existing CAH under the Necessary Provider replacement rules?
Critical Access Hospitals that were granted Necessary Provider designation prior to January 1, 2006, and choose to rebuild in a new location that does not meet the current distance requirements, are treated in the same manner as if they were building a replacement facility at the original location. In order to maintain CAH status and the necessary provider designation, the new facility must satisfy the following requirements:
- Meet the same criteria that led to its original state designation
- Serve at least 75% of the same service area
- Offer at least 75% of the same services
- Utilize at least 75% of the same staff in its new location
See the September 7, 2007, letter from CMS to state survey agency directors titled Critical Access Hospitals (CAHs): Distance from Other Providers and Relocation of CAHs with a Necessary Provider Designation for more detailed information.
Is there a limit on the length of stay for patients at CAHs?
Critical Access Hospitals must maintain an annual average length of stay of 96 hours or less for their acute care patients. The following are not included when calculating the 96-hour average:
- Time spent in the CAH as an outpatient
- Time spent in a CAH swing bed
- Time spent in a CAH distinct part unit (DPU)
How many beds are allowed?
CAHs may have a maximum of 25 acute care inpatient beds. For CAHs with swing bed agreements, any of their beds can be used for inpatient acute care or for swing bed services. Any hospital-type bed which is located in, or adjacent to, any location where the hospital bed could be used for inpatient care counts toward the 25-bed limit.
Certain beds do not count toward the 25-bed limit, including examination or procedure beds, stretchers, operating room tables, and beds in Medicare certified rehabilitation or psychiatric distinct part units. For a complete list of beds that do not count toward the 25 bed limit, please see Section C-0211, §485.620(a) Standard: Number of Beds: Interpretive Guidelines of the CMS State Operations Manual: Appendix W.
What is a swing bed?
A swing bed is a bed that can be used for either acute care or post-acute care that is equivalent to skilled nursing facility (SNF) care. The Centers for Medicare & Medicaid Services approves CAHs, and other hospitals, to furnish swing beds, which gives the facility flexibility to meet unpredictable demands for acute care and SNF care.
The Rural Monitor article History of the Swing Bed: A Look Through the Rural Rearview Mirror describes the evolution of the swing bed program to meet the acute and post-acute care needs of rural residents. Swing beds offer an alternative to skilled nursing facilities. This option may be useful in rural areas, which are less likely to have a stand-alone SNF. In addition, populations in rural areas tend to be older, and swing beds are well-adapted for treating health problems typically seen in aging patients. The most commonly reported need was for aging patients who require rehabilitation following their hospital stay, according to Why Use Swing Beds? Conversations with Hospital Administrators and Staff. Furthermore, swing beds help stabilize healthcare facilities’ census and may provide financial benefits. Swing bed services in CAHs are eligible for cost-based reimbursement, while swing bed services in non-CAH small rural hospitals are paid under the SNF prospective payment system.
For these reasons, swing bed post-acute care is common in rural healthcare facilities. According to Post-Acute Skilled Nursing Care Availability in Rural United States, 56% of all rural counties have at least one facility that provides post-acute skilled nursing care through a swing bed program.
For more details about the swing bed program, see the Medicare Learning Network: Swing Bed Services fact sheet and the Rural Monitor article Understanding the Rural Swing Bed: More than Just a Reimbursement Policy.
What emergency services are CAHs required to provide? What are staffing requirements for emergency services?
Emergency Department Services
CAHs must provide 24-hour emergency services.
Qualifying medical staff must be onsite or on-call and available onsite within 30 minutes at all times. Onsite response times may be extended to 60 minutes if certain frontier or remote area criteria are met.
The staff onsite or on-call must meet state licensure requirements. CAH Condition of Participation: Emergency Services specifies that coverage may be provided by a doctor of medicine (MD) or doctor of osteopathy (DO), a physician assistant, a nurse practitioner, or a clinical nurse specialist with experience and training in emergency care. Under temporary, limited circumstances, coverage may be provided by a registered nurse. In a June 7, 2013, memorandum, CMS clarified these requirements by stating that under CAH CoPs, an MD or DO is not required to be available in addition to a non-physician practitioner. Additionally, this requirement may be met in whole or in part through the use of an MD or DO via telemedicine.
As of October 1, 2007, CMS requires that any hospital, including a CAH, that does not have a physician on site 24 hours per day, 7 days per week, provide a notice to all patients upon admission. The notice must address how emergency services are provided when a physician is not onsite. For more information, please see page 47413 of the August 22, 2007, Federal Register notice, Medicare Program; Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Year 2008 Rates; Final Rule.
Emergency Medical Services
Unlike emergency department services, CAHs are not required to provide emergency medical services.
Characteristics and Challenges of Rural Ambulance Agencies – A Brief Review and Policy Considerations notes that unlike Critical Access Hospitals, ambulance services are typically not reimbursed at-cost. As a result, many CAHs are not inclined to maintain an ambulance service. According to Community Impact and Benefit Activities of CAHs, Other Rural, and Urban Hospitals, 2020, 22.4% of Critical Access Hospitals provided ambulance services in 2020. However, after accounting for the role of hospital health systems and joint ventures, 54.5% of CAHs had access to ambulance services. In addition, 47.8% of CAHs were designated as certified trauma centers.
The Frontier Community Health Integration Project (FCHIP) Demonstration, a joint demonstration project between the Centers for Medicare & Medicaid Services and the Federal Office of Rural Health Policy, reimbursed two participating CAHs 101% of reasonable costs of furnishing Medicare Part B ambulance services instead of being paid under the Medicare ambulance fee schedule. These CAHs utilized the funding to provide increased stipends to volunteer emergency medical technicians (EMTs), hold additional EMT training classes, and purchase equipment. Although FCHIP initially concluded in 2019, the Consolidated Appropriations Act, 2021, extended the program for an additional 5 years.
For more information on Emergency Medical Services in rural communities, see RHIhub’s Rural Emergency Medical Services (EMS) and Trauma topic guide.
What kinds of agreements does a CAH need to have with an acute care hospital?
As part of the agreements provision in the CAH Conditions of Participation, a CAH must develop agreements with an acute care hospital related to patient referral and transfer, communication, and emergency and non-emergency patient transportation. The agreement must include at least one other hospital that furnishes acute care services and can receive transfers of patients requiring services that are not available in the CAH.
The CAH may also have an agreement with its referral hospital for quality assurance, or choose to have that agreement with another organization. State networking requirements vary. For more information on quality assurance options, see What are the quality assurance and quality improvement options for CAHs?
Where can I find examples of CAH network agreements, tools, and other materials?
RHIhub’s Resources by Topic: Critical Access Hospitals lists hundreds of resources from organizations across the country. You can narrow the list by selecting resource type “Tool” for a number of financial and quality tools specific to CAHs.
The Arizona Critical Access Hospital Designation Manual provides samples of a:
- Rural Health Network Agreement (p. 23-27)
- Rural EMS Agreement (p. 28)
- Community Needs Assessment Template (p.31-33)
How do staffing and other requirements for CAHs differ from those of general acute care hospitals?
Under the Medicare Conditions of Participation (CoP), CAHs are granted greater staffing flexibility through two main provisions:
- Medical Staff
A Critical Access Hospital must have at least one MD or DO physician, but that person is not required to be onsite. Advanced practice providers, such as physician assistants, nurse practitioners, and clinical nurse specialists can be an independent part of the medical staff and can provide direct service to patients, including emergency services. - Nursing Staff
General acute care hospitals are required to have a registered nurse onsite 24/7. Federal requirements allow for CAHs to close, and therefore have no nursing staff on duty, if the facility is without inpatients. Additional requirements vary by state. For example, some states may offer flexibility by allowing an LPN to cover a shift in place of an RN when there are no acute patients. Contact your state survey agency for details.
CAHs must continue to meet their state licensure laws if those are stricter than the Medicare CoP.
Aside from staffing differences, requirements for CAHs and general acute care hospitals are very similar. CAHs must meet the requirements for the services they choose to provide. For example, if a CAH provides surgical services, it must meet the same relevant surgery requirements as a general acute care hospital.
Some issues may vary from state to state based on state licensure laws or other factors. To find out more about your state’s requirements, contact your State Rural Hospital Flexibility Program Contact.
Are Critical Access Hospitals eligible for the 340B program?
The 340B program allows certain eligible healthcare facilities to purchase prescription and non-prescription medications at reduced cost. Critical Access Hospitals that meet the eligibility criteria are able to participate in the 340B program as a Covered Entity. A 2018 report from the Government Accountability Office indicated that 77% of all CAHs participated in the 340B program in 2016 and accounted for 45% of all hospitals participating in the program that year.
See RHIhub’s Rural Pharmacy and Prescription Drugs topic guide for more information about the 340B program.
What sources of capital funding exist for CAHs?
Critical Access Hospitals (CAHs) qualify for a variety of capital funding opportunities, such as grants and loans. Among others, the following two federal programs focus on helping CAHs with their capital funding needs:
- USDA Community Facilities Loan and Grant Program – Provides funding to construct, expand, or improve rural healthcare facilities, including CAHs.
- HUD Section 242: Hospital Mortgage Insurance Program – Helps rural healthcare facilities finance new construction, refinance debt, or purchase new equipment such as hospital beds and office machines.
Visit the funding section of this guide and the Capital Funding topic guide for additional opportunities and information.
What is the CAH survey process?
A facility interested in CAH status should contact its state survey agency to request application materials. The state agency will review and forward the application to a CMS regional office. The CMS regional office will authorize a survey, and the state agency will then contact the facility to arrange a survey date. The survey will verify that the CAH meets the federal facility requirements. Details about the survey process are available in Appendix W of the CMS State Operations Manual.
A facility will also need to be recertified by the state survey agency on a schedule consistent with the survey guidelines issued by CMS each year. A facility may be decertified if a situation or issue presents immediate jeopardy and is not resolved quickly. Details about the recertification process are in Chapter 2 of the CMS State Operations Manual.
Additionally, facilities may obtain deemed status if accredited by a CMS-approved Medicare accreditation organization. In the case of a deemed provider, the state agency does not conduct an initial survey. While the facility seeking deemed status must still contact the state agency to acquire the Medicare and/or Medicaid certification materials, initial certification and subsequent recertification is performed by the accrediting organization. CMS maintains a list of Approved Accreditation Organization Contacts for Prospective Clients. The following accreditation organizations are approved for CAH certification:
- DNV GL – Healthcare (DNV GL)
- The Joint Commission (TJC)
What legislation has affected the Critical Access Hospital program?
According to the American Hospital Association, several pieces of legislation have modified the Critical Access Hospital (CAH) program since its creation through the Balanced Budget Act of 1997. The following legislation are integral to the Critical Access Hospital (CAH) program:
- Balanced Budget Act (BBA) of 1997
Created the CAH program, outlining all details of the program including eligibility and operational regulations. - Medicare, Medicaid, and SCHIP Balanced Budget Refinement Act (BBRA) of 1999
Corrected unanticipated adverse payment and regulatory consequences of the BBA of 1997. - Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act (BIPA) of 2000
Provided further exemptions and reimbursement improvements to CAHs, which strengthen the overall program. - Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003
Enhanced CAH payments, expanded bed-size flexibility, provided continued funding for the Medicare Rural Hospital Flexibility (Flex) Program grants, and increased Medicare payments to 101% of reasonable costs. It also enacted a sunset of the necessary provider provision, effective January 1, 2006. - Medicare Improvements for Patients and Providers Act (MIPPA) of 2008
Further expanded Flex grants, and allowed CAHs to receive 101% of reasonable costs for clinical lab services provided to Medicare beneficiaries even if the specimen was collected offsite or at another CAH-operated facility. - American Recovery and Reinvestment Act (ARRA) of 2009
Created several grant, loan, and incentive programs to support the adoption of new health information technology (HIT) in CAHs. - Patient Protection and Affordable Care Act (ACA)
Included several efforts aimed at reducing workforce shortages, such as expanding Area Health Education Centers (AHECs) and further investing in the National Health Service Corps. It also allowed CAHs to participate in the 340B program, making reduced cost pharmaceuticals accessible in rural communities. - Budget Control Act of 2011
Imposed mandatory across-the-board reductions in federal spending to achieve $1.2 trillion in budget savings over a 10-year period (also known as sequestration). - Bipartisan Budget Act of 2013/Pathway for SGR Reform Act of 2013
Extended sequestration for an additional two years (2022 and 2023) beyond the period specified in the Budget Control Act of 2011 at the same percentage of spending. The Bipartisan Budget Acts of 2015 and 2018 extended sequestration through 2027. The Coronavirus Aid, Relief, and Economic Security (CARES) Act further extended sequestration through fiscal year 2030. However, the CARES Act also paused sequestration amid the COVID-19 pandemic, and legislation passed in April 2021 extended the pause through December 2021.
RHIhub’s Rural Health Policy guide provides additional information on policies and legislation affecting rural healthcare.
What are Rural Emergency Hospitals?
The United States Congress established the Rural Emergency Hospital (REH) as a new Medicare provider type in the Consolidated Appropriations Act, 2021. Effective January 1, 2023, this law will allow Critical Access Hospitals and other small rural hospitals meeting eligibility criteria to convert to Rural Emergency Hospital (REH) status. REHs will be reimbursed at 105% of the outpatient prospective payment system (OPPS) for emergency and outpatient care services in addition to a fixed monthly payment. Unlike Critical Access Hospitals, REHs will not be allowed to provide inpatient services.
For additional information on Rural Emergency Hospitals, including eligibility criteria, staffing and service requirements, and technical assistance resources, see the Rural Emergency Hospitals topic guide.
Who can answer questions about CAH status or reimbursement issues?
Your State Rural Hospital Flexibility Program Contact can provide ongoing guidance about CAH issues. Other important contacts include:
- CMS Regional Office Rural Health Coordinator – for questions about CMS regulations
- State Survey Agency – for survey and certification questions
- National Rural Health Resource Center’s Technical Assistance and Services Center (TASC) – for technical assistance, information, and other resources
- Medicare Administrative Contractor (MAC) – for questions about Medicare claims, reimbursement, and billing issues

