Telehealth: A Path to Virtual Integrated Care
Telehealth’s Role in Digital Transformation
Telehealth is part of a larger digital transformation in healthcare. Care that used to take place only in brick-and-mortar settings can now occur digitally. Accordingly, hospitals and health systems are exploring a variety of virtual care models, many of which are underpinned by telehealth technology.
Hospitals already are using telehealth to improve access and fill gaps in care, provide 24/7 service, and expand access to medical specialists. As demands for healthcare services increase, telehealth offers a smart way to leverage finite healthcare resources. Telehealth and digital healthcare enable a model of care that is more affordable and integrated into patients’ lives. Hospitals and health systems that are working to increase the maturity of their telehealth capabilities will be well-positioned to meet patient demands for digital tools that allow them to conveniently engage in care.
Defining Telehealth Delivery Platforms: Provider to Provider and Direct to Consumer
Telehealth delivery platforms fall into two main categories:
- Provider to provider extends expertise and resources for specialty and subspecialty care and addresses workforce shortages and the efficient use of health professionals.
- Direct to consumer includes virtual care, remote patient monitoring and extending care delivery into the home via technology.
The most common telehealth platforms include both synchronous and asynchronous technologies, such as videoconferencing, store-and-forward imaging, email and remote patient monitoring.
9 Areas in Which Telehealth Is Expanding Access
One of the most frequent reasons hospitals use telehealth is to extend access to specialty care. By increasing access points and redistributing expertise where it’s needed, telehealth can address disparities and improve outcomes, from pediatric health services to senior care. Telehealth platforms can be used effectively to provide the following services:
- Pharmacy services, including patient counseling, medication review and prescription verification, for patients with chronic diseases
- Chronic care management, recording vital signs through home-monitoring systems and sending alerts to clinicians when readings fall out of the normal range
- Telestroke services, creating access to the limited supply of stroke neurologists and targeted use of therapies that preserve brain function and save lives
- Tele-ICU tools, providing 24-hour intensive support to deliver optimal local care to the most acute patients
- Specialty telemedicine consults, addressing challenges patients face when accessing specialty care services, such as transportation, eligibility, translation and cultural competency
- Diagnostic screening for diabetes-related eye disease, increasing the number of diabetes patients who receive eye exams, which are 90% effective in preventing blindness
- Sleep disorders, monitoring patients with sleep apnea for sleep patterns, body positions and breathing
- Telepsychiatry, assisting patients in need of behavioral health services
- Opioid use disorder (OUD), expanding access to medication-assisted treatment (MAT)
Challenges to Widespread Telehealth Adoption
There are several barriers to expanding access to care through telehealth. The eight most significant hurdles are:
- Restrictions on how Medicare and other payers cover and pay for telehealth
- Licensure laws and regulations that limit the ability to provide telehealth services across state lines
- The lack of adequate broadband services in some areas to support telehealth
- The lack of leadership and organizational commitment to develop an overarching strategy and integrate care delivery
- Decentralized departmental solutions and pilot programs without governance structure and dedicated management
- The high cost of technologies and infrastructure and a lack of funding
- Inadequate clinical engagement and readiness without consideration of human factors in the user experience and of workflows for both clinicians and patients
- Evolving measures of success and key performance indicators (KPIs) hampering scaled platforms
Why Telehealth Is Critical to Health System Transformation
Using telehealth tools to treat patients is a more effective and efficient way to use limited staff and resources. Regional growth can be leveraged across sites of care through telehealth networks. Virtual care technology can improve the timing, quality and impact of care for more patients by eliminating travel and bringing in specialized care, as needed. An enterprise approach to virtual care creates staffing efficiencies and specialist capacity, improves access and convenience for patients, and lowers the cost of care.
To advance the adoption, sustainability and optimization of telehealth services, a maturity model is useful to set criteria for competency, capability and level of sophistication. The Hospital Telehealth Maturity Model developed by Manatt Health (see Exhibit 1) provides a framework that can be used to measure and develop existing and prospective telehealth services by program and platform within prescribed best-practice parameters. The model may be useful for self-assessment and benchmarking to guide telehealth programs toward adopting best practices.
Exhibit 1:
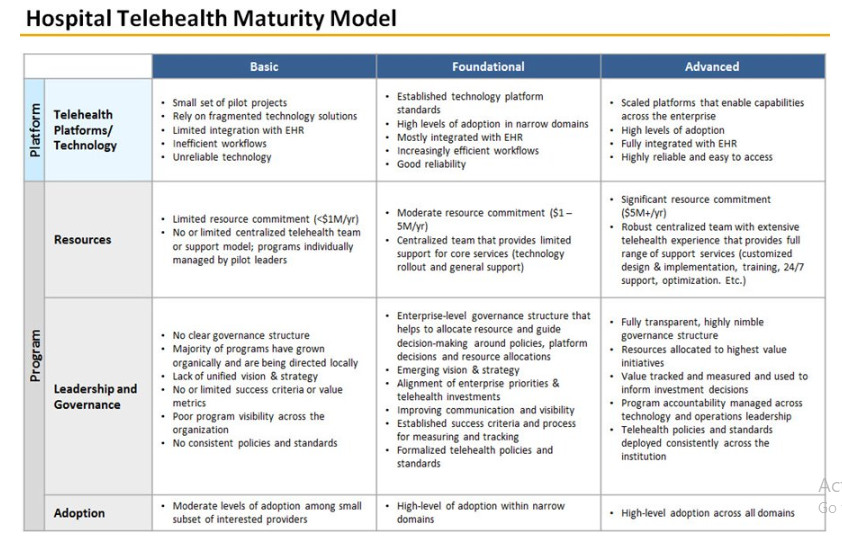
Hospitals and health systems use telehealth in different ways to address patient needs and organizational strategies. Using 2017 AHA Annual Survey Data on the adoption and use of telehealth, the AHA Center for Health Innovation has prepared peer comparison data for community hospitals, health systems, academic medical centers, urban hospitals, rural hospitals and critical access hospitals. Findings show that:
- Community hospitals are moving from the basic to the foundational level on the Hospital Telehealth Maturity Model with opportunities to address gaps in care. Seventy-six percent have a computerized telehealth system.
- Many health systems are moving from the foundational to the advanced level on the Hospital Telehealth Maturity Model with opportunities to gain further efficiencies by scaling opportunities across the enterprise. Eighty-nine percent have a computerized telehealth system.
- Academic medical centers are moving from the foundational to the advanced level on the Hospital Telehealth Maturity Model with opportunities to use resources more efficiently and leverage their deep expertise. Ninety-one percent have a computerized telehealth system.
- Urban hospitals are moving from the basic to the foundational level on the Hospital Telehealth Maturity Model with opportunities to address gaps in care and care coordination across the continuum. Seventy-seven percent have a computerized telehealth system.
- Most rural hospitals are at the basic level on the Hospital Telehealth Maturity Model with opportunities to address gaps in care. Seventy-eight percent have a computerized telehealth system.
- Most critical access hospitals are at the basic level on the Hospital Telehealth Maturity Model with opportunities to address gaps in care and expand the provider network. Seventy-eight percent have a computerized telehealth system.
How Hospitals and Health Systems Can Build Their Telehealth Capacity
How do hospitals and health systems move up the maturity continuum? It starts with culture—and culture starts at the top. The governing board and C-suite can ignite cultural change with a telehealth vision statement that embraces virtual care as an extension of what the hospital or health system already does, rather than as something new or different.
In fact, mature hospitals and health systems prefer the term virtual care to focus on the experience rather than telehealth, which many people associate with technology. Physicians are more accepting of virtual care as a new form of care than they are of new technologies. Succeeding in telehealth is as much a change in mindset as it is a change in technology and vendors.
Scaling and Optimizing Telehealth Programs
The two essential elements of a successful telehealth program are integration into the electronic health record (EHR) system and integration into clinicians’ workflows. Other essential elements for successful optimization include:
- Using community and patient needs as the starting points for the consideration of new telehealth services
- Using telehealth services to coordinate care across healthcare settings
- Incorporating telehealth services into value-based care
- Using telehealth services to help direct patients to the appropriate level of care
- Setting KPIs for telehealth
Successful hospital and health system telehealth programs require discerning technology choices and critical vendor selection. Success also demands uncomfortable cultural changes and the right executive to create a comprehensive virtual care delivery system for patients.

