CMS Proposes Telehealth Updates to the 2021 Medicare Physician Fee Schedule
On August 3, the Centers for Medicare & Medicaid Services (CMS) released its proposed Medicare Physician Fee Schedule (MPFS) updates for the 2021 calendar year, addressing among other policy changes how CMS will treat telehealth codes for the duration of and following the COVID-19 public health emergency (PHE).
Background: CMS’ Process for Reviewing New Telehealth Codes
CMS permits any interested party to submit a request to add services to the list of codes covered by Medicare when furnished via remote practice. CMS reviews these requests to determine whether the telehealth service will be added in a subsequent MPFS rulemaking, and in doing so assigns each requested service to one of two categories. Services that are viewed as similar to existing approved telehealth codes (such as professional consultations and office visits) are reviewed on a “category 1” basis, while those services not similar to the current list fall into “category 2.” CMS reviews category 2 requests in light of whether the use of remote technology to deliver the service demonstrates a “clinical benefit” to the patient.
In response to the PHE, CMS and other federal agencies have taken a series of actions to waive otherwise-applicable restrictions on the use of telehealth modalities to deliver, and be reimbursed for, patient care during the pandemic. On March 31, CMS issued an Interim Final Rule, expanding Medicare coverage for more than 80 new telehealth codes for the duration of the PHE. These services were added on a category 2 basis, and include emergency room, discharge and home visits, even if the beneficiary’s communications system has only audio (and not video) capabilities. Subsequently, on May 1, CMS expanded the list on a sub-regulatory basis (as opposed to via rulemaking) to include still more telehealth services as recommended by the public or identified internally.
Telehealth in the 2021 Proposed MPFS
CMS’ proposed policy updates specific to Medicare reimbursement for telehealth are summarized below. CMS will consider stakeholder comments to the proposed rule received any time before 5:00 p.m. Eastern Time on October 5, 2020.
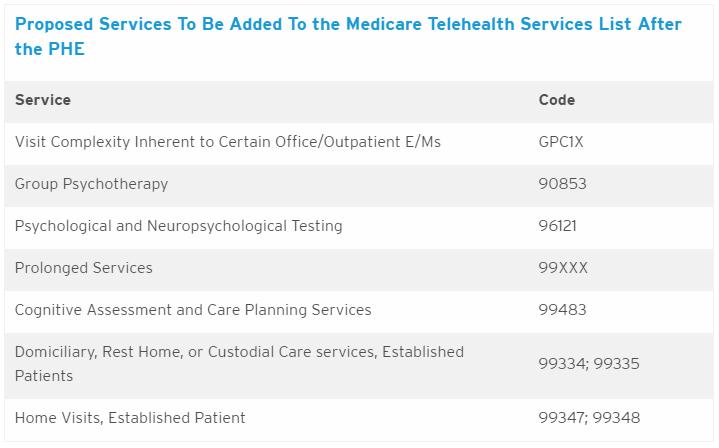
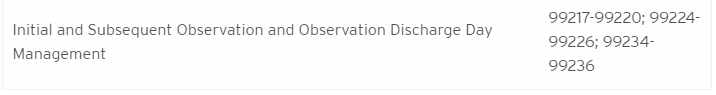
- CMS proposes to keep certain codes on the approved telehealth list even after the PHE is over, on either an interim or permanent basis. These codes, added on a category 1 basis because CMS finds they are “sufficiently similar to services currently on the Medicare telehealth services list,” include the following:
- CMS has declined to propose adding HCPCS Codes 96040 and S0265 (medical genetics) to the list of approved telehealth codes.
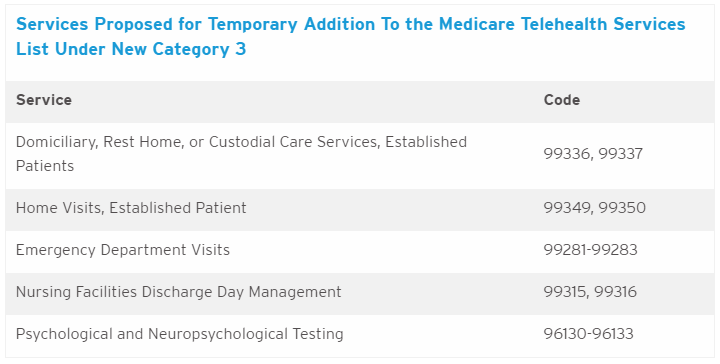
- Recognizing the likelihood of a gap between the termination of the PHE and any subsequent rulemaking period for the addition of telehealth codes to the MPFS, CMS proposes to create a third category of criteria for adding services to the list of telehealth codes. Services in this “category 3“ would be those that were added during the PHE and for which there is likely to be a clinical benefit when furnished via telehealth, but for which there is not yet sufficient evidence to consider the services permanent additions on a category 1 or category 2 basis. To be permanently added to the list of Medicare-reimbursable codes, these category 3 services eventually must meet the criteria under category 1 or category 2. Any service added under this new third category would remain on the list through the calendar year in which the PHE ends. CMS proposes to include the following codes in category 3:
- CMS is seeking comment on whether any of the above services should be considered as category 3 temporary additions or whether services currently not proposed should be considered.
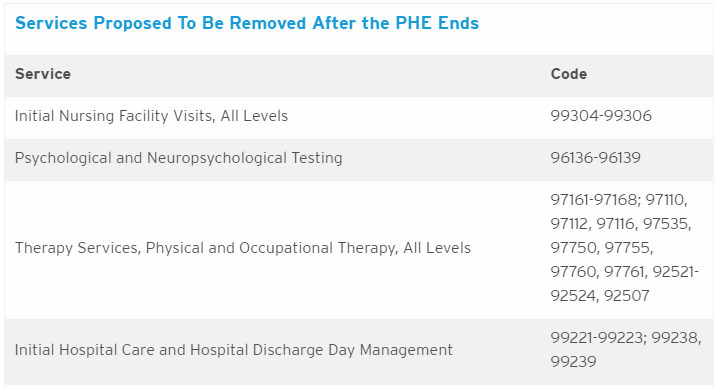
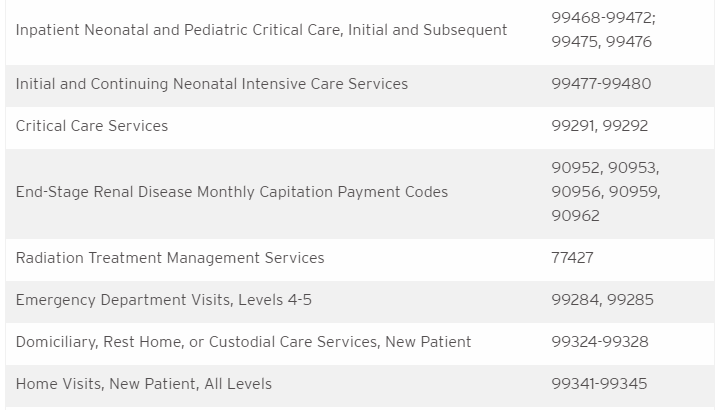
- The proposed MPFS would not retain certain telehealth codes following the termination of the PHE as CMS has not identified sufficient information to demonstrate clinical benefit outside the circumstances of the pandemic. However, CMS is requesting comment on whether any of these services should be added on a temporary, category 3 basis.
CMS proposes additional updates to telehealth reimbursement in this rule, including the following:
- In the March 31 Interim Final Rule, CMS permitted separate payment for audio-only telephone E/M visits. CMS has not proposed to continue payment for these services after the PHE ends because it cannot waive the requirement that telehealth services be furnished using an interactive system that includes two-way, audio-video communication technology; however, CMS is seeking input on whether this flexibility can remain in place on a provisional basis. CMS recognizes the benefit for audio-only interaction to allow beneficiaries to avoid possible sources of infection, and therefore is seeking input on whether it should develop coding and payment for services similar to the “virtual check-in.”
- CMS proposes to extend its PHE flexibility which allowed direct supervision to include the virtual presence of a supervising physician using audio-video real-time communications technology. CMS also clarifies that if a physician is using a virtual presence for direct supervision, it is sufficient for the physician to be immediately available to engage via audio-visual technology. The extension would last until the later of either the calendar year in which the PHE ends or December 31, 2021.
- Historically, initial and periodic visits from a physician or non-physician practitioner were required to be conducted in-person for residents of skilled nursing facilities. During the PHE, CMS waived the in-person requirement and allowed these visits to be conducted via telehealth. Pursuant to the proposed rule, CMS is soliciting comments on whether this flexibility should be maintained on a permanent basis.
- CMS proposes removing its position that telephones, facsimile machines and electronic mail systems do not meet the definition of an interactive telecommunications system.
- In recent years, CMS has made separate payment for a number of services that use telecommunications technology but are not considered Medicare telehealth services (e.g., remote patient monitoring, virtual check-ins). CMS is seeking comment on whether there are additional services that are not technically “telehealth” services (and, therefore, would not need to be added to the Medicare telehealth services list in order to be reimbursable when furnished using telecommunications technology).
- CMS proposes to clarify that services that may be billed incident-to may be provided via telehealth incident to a physician’s service and under the direct supervision of the billing professional.

