Comparing 11 top telehealth platforms: Company execs tout quality, safety, EHR integrations
Leaders in the telemedicine space explain and compare their technology services and modalities.
August 2, 2017 by Bill Siwicki
Telemedicine is on the rise, just ask the companies behind the technology.
“We’ve had more telehealth visits during the last year than in the nine previous years combined,” said Katie Ruigh, senior vice president of product at telemedicine technology vendor American Well. “In terms of clients, we have about 70 health systems using our platform, and we had half that at the end of 2015.”
Currently, 31 percent of healthcare organizations use video-based telemedicine services and 34 percent offer remote patient monitoring, according to a KPMG survey conducted by HIMSS Analytics. Expansion plans for these services will drive future use with another 44 percent of healthcare organizations eyeing video-based telemedicine services and 48 percent planning for remote patient monitoring, the survey of 147 C-suite, IT and clinical leaders found.
“The business case for implementing a virtual care program is improving as healthcare evolves toward value-based care incentives from limited fee-for-service reimbursements,” said Richard Bakalar, MD, KPMG managing director and member of the firm’s Global Healthcare Center of Excellence. “It’s more efficient for high cost and limited clinical staff as well as other onsite resources, while making it more convenient and timely for patients to receive their care.”
In this guide, we gave executives from 11 telehealth company’s a chance to talk about what their products offer and how they are attempting to help healthcare providers gain a stronger expertise with their telehealth solutions.
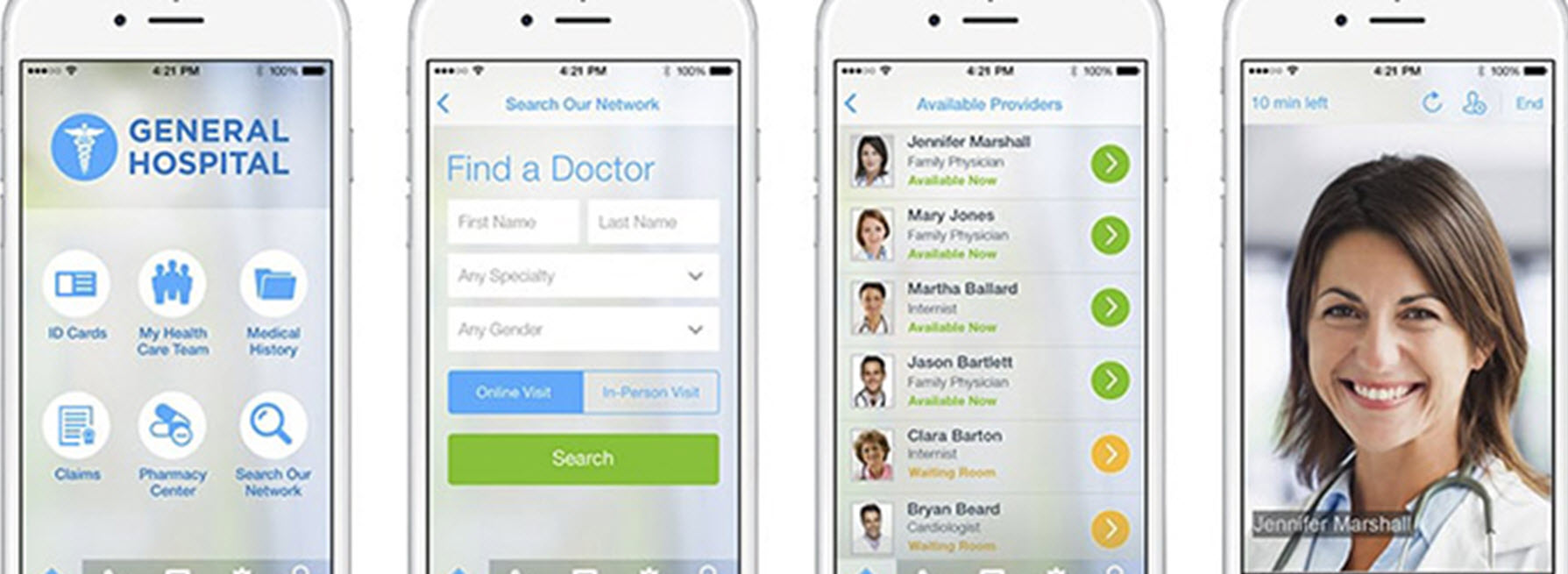
American Well
American Well offers telehealth visits by video and phone, though the vast majority are video. The vendor supports patient-to-provider, provider-to-provider and multi-party video visits as well as service lines and practices that enable healthcare organizations to customize the telehealth experience for their providers and patients. Organizations can brand a service, a specialty or a facility, and have a different look and feel or workflow for each of the service lines.
“With the virtual visit itself, there is another bucket of capabilities around medical history collection and teeing up a visit,” said Ruigh. “We collect self-reported data from the patient like medical history and biometric information and vital signs. So, for instance, with our Apple Health integration they can use their devices in-home and we’re able to pull that data in and make it available for the consult. And we also can pull data from external sources like from an EHR system or from pharmacies.”
“…If they want to pass a subset of clinical information like a problem list from an EHR, they can pass it to the American Well platform. And after that, if any documentation occurs on our platform, we can pass that data back to the EHR.”
American Well wants to set up every virtual visit with the appropriate clinical context from a variety of different sources so physicians can treat patients as if they were in the same room together.
“How would a provider virtually treat a patient,” Ruigh said. “They treat a patient as if they were in person, including diagnosing them clinically, assigning any procedures, prescribing, writing clinical notes; as the providers see the patients they can do the same things they would do in a brick-and-mortar setting. And if they document using the American Well platform, that documentation can get back into the system of record. And we offer secure messaging – here a patient and a provider can communicate in a secure fashion like emails but because it is on our platform it’s secure and HIPAA-compliant.”
American Well claims its telemedicine exchange is a unique product. It’s a collection of providers ready and able to deliver consults from different provider organizations.
“The exchange is a way for our clients who own and operate telehealth solutions to share clinical services with one another, or to access clinical services from another American Well partner,” Ruigh said. “We have a lot of clinicians who are using telehealth with their own patients and want to use it as a way to capture new patients. Cleveland Clinic has made their services available through an American Well system, and people can see Anthem’s white label version of the American Well technology.”
Samsung also recently partnered with American Well, integrating virtual visits into the Samsung health experience app.
American Well says its products can be integrated with EHRs, too.
“We have a suite of APIs,” Ruigh said. “We have a scheduling integration so they can register on their side and pass that visit to us. And from a clinical perspective, we have an inbound/outbound clinical integration option. So if they want to pass a subset of clinical information like a problem list from an EHR, they can pass it to the American Well platform. And after that, if any documentation occurs on our platform, we can pass that data back to the EHR. And that data is passed as discrete data, not just a PDF or a screen shot, it takes the data and puts them into the right places in that EHR system.”
Avizia
Avizia’s technology enables patient access to clinicians, provider collaboration from the onset of a condition, care coordination, and point-of-care devices. The solution includes carts and tablets as well as proprietary software that enables remote consultations with patients using devices of their choosing.
“I would not say we have one predominant service line or specialty area,” said Chief Marketing Officer Tycene Fritcher. “I would say right now we are more comprehensive, which is a blessing and a curse. Because I cannot say I am the leader in tele-stroke today, but we have taken that stance in the market where we want to be that comprehensive provider, so we are OK not leading in one area, we want to be the predominant health system telehealth solution provider.”
Fritcher said it’s the company’s care coordination that sets it apart.
“It’s no secret that originally Avizia started as a point-of-care device company, started with carts and so forth, but we liked the path of our carts being platform-agnostic,” Fritcher said. “When we added in our solution set, we wanted to enable greater care coordination. So integrating with an EHR. And care coordination enabling instant alerts as opposed to the old phones, paging physicians, or emailing or texting them.”
When a caregiver clicks on a secure instant alert link saying a consult is waiting, they instantly are immersed in case details and can connect to that telehealth video visit.
“Some of the chief pain points health systems are looking to address are reduced costs with increased access and improved outcomes, and face-to-face allows them to do that in a significant way,” Fritcher said. “Face-to-face enables a higher level of revenue than the methods of telehealth that are just voice.”
Avizia’s telemedicine technology can be used on any desktop, laptop or mobile device with a web browser and a camera. As for its telemedicine carts, the video infrastructure here could be one a healthcare organization already has in place, or Avizia’s video cloud technology, which is designed to help organizations avoid infrastructure costs.
The company said its technology meets all HIPAA compliance requirements and uses end-to-end encryption. Further, the company continuously monitors for suspect traffic patterns and fraud attempts.
“We are a cloud-based application, and we use Amazon Web Services,” said Cory Costley, chief product officer. “We go through rigorous testing by third parties and others to do intrusion detection, we have robust service providers, we sign business associate agreements, those are all set up to make sure things are as secure as possible. We have active and passive intrusion detection inside of the network and regular audits to ensure things are safe and secure.”
Avizia integrates with EHRs, from standards-based data exchange like HL7 to custom API integration.
Carena
Carena, which started as a primary care company that delivered care by house calls ,has its white label telemedicine technology in more than 120 U.S. hospitals, the company says.
“When we moved into telemedicine, our approach was how do we deliver as much of that value and patient experience as a house call but virtually,” said Ralph Derrickson, president and CEO. “The way we deliver our services today is we build virtual clinics for health systems. A virtual clinic is a way for a patient to come to a health system without knowing what they need, they just need help. We operate that virtual clinic, we provide the software to present that to the patient, the software tools so providers can communicate with those patients, and the back-end software and systems to integrate the activity in the virtual clinic into the rest of their health system.”
Carena also provides the medical staffing so the care in the virtual clinic is an on-demand service offering.
“Health systems do everything via schedules, they are not set up to do on-demand,” Derrickson said. “We provide 24/7 on-demand service and staffing, which is quite different than a lot of telemedicine providers. We have a network of providers that are employed by our medical groups, their adherence to clinical guidelines are substantially different from the rest of the market. We provide operating support, we stand it up and operate it for them. They can outsource it to us, we also provide the digital marketing services to drive utilization.”
A virtual clinic asks patients for the least amount of information possible to reduce the click-to-care time, the company said. It can support multiple video formats, including Skype, Apple Facetime and built-in video. Patients indicate how they wish to pay and consent to treatment after entering minimal health information, all of which takes about five minutes, the company said.
Patients could be people a virtual clinic knows nothing about, a member in a membership plan or part of a managed at-risk population.
“On average a patient will wait less than 10 minutes; maybe 15 minutes,” Derrickson said. “They will be notified when the provider arrives in the virtual exam room in whichever video format they choose. Our visits last 20 minutes, we do a full history, we make sure we can treat them, if not we refer them to an urgent care center or encourage them to wait for their regular doctor if appropriate. When that visit is done, they receive a visit summary, any treatment information that the physician is giving, follow-up information if the patient needs additional treatment, then give them information on the follow-up care, and if there was a prescription that prescription is sent to the pharmacy of choice.”
Clinical information is shared with the health system, and if the patient indicates a primary care provider, the information goes directly to them, as well. Carena does integrations directly into EHRs; some health systems will have more sophisticated integrations while others will use a CCDA or PDF, the company said. The billing staff is billed. And if a patient was part of an at-risk population, Carena will notify care coordinators, as well.
The company said its telemedicine visits are secured by multi-factor authentication and end-to-end encryption of data at rest and in flight. Video services that patients may choose to use such as Facetime and Skype have their own sets of security in place.
“Offering virtual care, about 70 percent of the patients are new to a health system and that health system wants to start building a relationship with the patients so when they need medical care down the line they will come back,” Derrickson said.
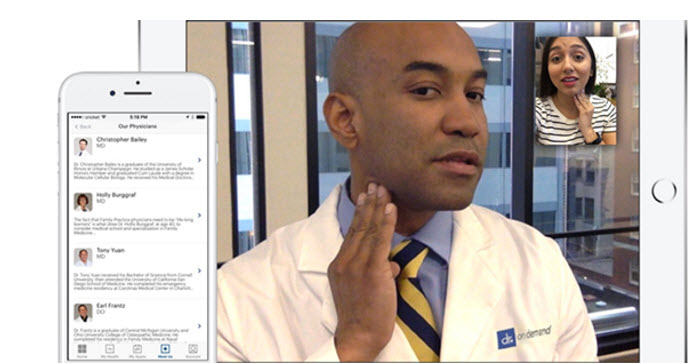
Doctor On Demand
Doctor On Demand views itself as a nationwide medical practice connecting consumers with board-certified physicians in an on-demand fashion. Consumers can gain access to a provider within minutes on a mobile device or a desktop or laptop with a camera. The company only offers video visits because the physician conducts a visit in the same way as he or she would in a brick-and-mortar setting, with a history, examination and treatment plan.
“We have done the closest approximation to that in-person visit, and the success rate we have with video is a major component of that,” said Ian Tong, MD, chief medical officer. “We were the first to develop the video technology that has the success rate of a cell phone call; we have a 98 percent success rate with video calls, and that is a very big technical achievement.”
Doctor On Demand offers access to a wide variety of types of physicians, including internists, family practitioners, pediatrics and emergency medicine providers; it also has a mental health practice.
“A lot of our competitors are communicating with patients through technology but saying we will call you back when we can find a provider for you,” Tong said. “We have a workforce of employed physicians who are on dedicated shifts, trained through our training programs, and who know the requirements and expectations of a video visit, and are trained for that visit, and are ready and on a dedicated shift so when that patient calls they have an average wait time of less than five minutes.”
Tong added that the company has high provider engagement in the training program and high provider satisfaction, adding that happy doctors practice better medicine.
“So it really allows us to provide a certain amount of customization of what we can offer,” he said. “So if a health system wants to offer a specific type of program, they want the mind/body approach to smoking cessation, our practice can offer that because we have the different providers set up and we can design an integrated medical practice for their patients.”
Providers and patients can connect with a mobile device or a desktop or laptop with a camera. Participants can access the system through a web browser or through Apple or Android mobile apps. The company also issues laptops to its providers so it can have a firm hold on security and authentication. The company has been certified for security by HITRUST.
Doctor On Demand has the capability to integrate with EHRs, but it is not something it stresses.
“We can do it; it’s a lot easier for us to do unidirectional, but we have done integration with one of the most complex EHRs out there, Epic,” Tong said. “It’s a capability we have demonstrated, but right now what we have found is if I talk to a health system or smaller practice, they do not want to invest in that area, each one of those is custom and it’s a big lift to do it and it’s expensive.”
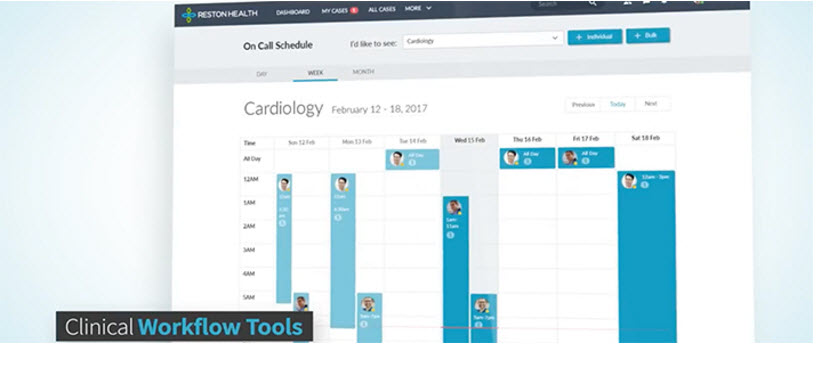
MDLive
MDLive’s telemedicine system offers a patient experience, a provider experience and a call center. A patient can come in through the mobile app, through a website or through the call center. The call center is for a phone-only visit. If a call center patient ultimately needs a video consult, call center staff guides them through downloading the mobile app or sends them to a URL to log in through a browser.
On the provider side, physicians log in to a dashboard where consultations are sourced one of two ways. Some consultations happen on-demand, where a patient comes in and will just drop themselves into the virtual waiting room. An algorithm in the background determines which patients to grab for physicians based on the state a patient is in, the licenses the physician has, and more information.
“The connection has HIPAA-compliant security and privacy controls in place, and we use end-to-end DTLS encryption.”
Physicians also have the ability to make themselves instantly available online so when a consumer comes through the front door they will see a list of providers and see that provider is available.
Further, physicians can create schedules for when they are available for consults, and patients can schedule their video consultations.
The provider on their dashboard sees medical history, surgical history, family history and anything the patient has entered into their consumer experience. The physician can also see data that might have been pulled in from a health plan claim file or an outside EHR integrated into the system.
“For Humana, whenever a Humana patient comes in to see one of our providers, our system has the integration built in to immediately recognize that the consumer belongs to a Humana plan and our system automatically goes out to the Humana system and brings the patient’s most recent health summary into the MDLive provider portal so the provider has the most recent data on that patient prior to seeing the patient,” said Brian Lichtlin, chief technology officer. “The physician can prepare himself with the history of that patient. Once they review that, they click another button and it connects them into the consultation.”
MDLive gets patients from three verticals: employers, health plans and health systems. Employers send eligibility files that say their employees are eligible along with some information on that patient. A health plan will push the subscriber ID for the plan so MDLive can determine who that person is and what their benefits are, along with some basic information. In both cases, patients fill out a digital clipboard with background information they want providers to see.
MDLive also gets telemedicine patients through an agreement with Walgreens, where Walgreens customers can see a doctor through MDLive video technology.
“When it comes to security, a consultation is treated with the same attention and confidence as a face-to-face visit,” Lichtlin said. “The connection has HIPAA-compliant security and privacy controls in place, and we use end-to-end DTLS encryption.”
And MDLive does integrate with EHRs.
“Some of the EHRs are very technically advanced. Folks like athenahealth, we connect to them through end-point APIs, they are on the cutting edge. Epic is starting to allow API integration, as well. We have a team of people who have been working in this business for the last 20 years, so we do all sorts of integrations. Some of your older EHR vendors are not deploying mobile end-points to integrate with so we do a lot of HL7 integration with the legacy EHRs.”
Philips
Philips delivers enterprise telehealth systems across multiple modalities in the hospital and in the home. The most critical patients are those in the ICU, where Philips has a specialized system that can be extended into med-surg floors and skilled nursing facilities. In the ambulatory setting, the company has systems to monitor patients in their homes and a suite of products to manage wellness and early stages of chronic illnesses.
Last summer Philips acquired Wellcentive, which helps providers entering value-based contracts maximize their outcomes and payments under those contracts. Those capabilities will be applied to Philips’ telehealth programs so Philips can recommend which patients would most benefit from telehealth and calculate the value that telehealth interventions will provide.
“We have a stroke module within our care management platform that allows folks into the telehealth center that act to manage the care the stroke patients get once they are in the emergency department,” said John Ryan, senior director, global marketing, at Philips telehealth. “We’ve used carts in skilled nursing facility settings to manage at-risk patients there. But our bread and butter to date has been the tele-ICU solutions. Clients start there and extend it from there into other solutions within the inpatient enterprise.”
In the inpatient setting, Philips has a database of 3.5 million patient records that it uses to develop algorithms that act on the signals coming in from patients so Philips can prioritize the patients for the care teams.
“On the ambulatory platform, one very unique differentiation is the fact that we can serve up assessments to patients in 33 different languages, and when those assessments come back to the clinician they can all come back in English,” Ryan said. “So if you are looking at population health management solutions in L.A. you can serve patients in Spanish or Farsi or Chinese. That form of communication is really important so you can apply your standards of care no matter where people originate from in the world.”
For the tele-ICU setting, hospitals need a video infrastructure for high-fidelity video connections. Additionally, there need to be interfaces to the EHR, as well as the various monitoring devices in the patient rooms.
“A lot of times you go in and it’s a very heterogeneous environment,” Ryan said. “Philips can work in these environments because we’re not coming at it from the EHR side, we know it’s a complex world and we’re used to coming in for one view of these patients.”
On the ambulatory side, providers use a desktop computer and patients use Philips devices, including a tablet, in the home for security and reliability, the company said.
“We are a class 2 medical device on the inpatient and ambulatory sides, we hold ourselves to a very high standard of reliability when it comes to the safety of information,” Ryan said.
Philips integrates with EHRs, which it considers critical to telehealth.
“On the ambulatory side we will take patient records down from the EHR, patient demographic information, medical record number, phone number, anything else pertinent to set up on the system, and then publish information like vital signs and assessments and notes back up into the medical records,” Ryan said. “The EHR tends to be history of what has happened with the patient. Telehealth tends to look at what is going to happen with the patient if you do not intervene. Any time the information is pertinent and collected it is published back up.”
Polycom
Polycom touts its high-quality audio and video and its content communication capabilities on various platforms, from a basic codec that one hooks up to a TV to a rolling cart that moves from room to room to things like tele-psychiatry on a desktop. In addition to these codec systems, Polycom also has software-enabled systems, such as mobile software for iPads and Android devices, as well as software for Macs and PCs, all with the ability to provide up to HD video. Polycom also offers APIs that other vendors can use to integrate Polycom software into their systems.
One of the top telemedicine areas for Polycom systems is stroke assessment, where there is a risk because of the limited time to dispense drugs to inhibit a stroke from doing further damage.
“In the case of tele-psychiatry, it is extremely important that a patient feels more than just comfortable, it has to be virtually equal to an in-person experience with a natural conversation both from an audio and video perspective.”
“A patient might be in the middle of Kentucky but need access to a center of excellence, for example, in Louisville, to talk with a doctor who can make that assessment, and it’s critical for the doctor to be able to see and hear the patient clearly and make it easy for the technicians on the end to control the camera and zoom in and see if the face is drooping and make that clinical diagnosis remotely,” said Bob Knauf, senior product marketing manager.
Polycom is seeing a lot of growth in the field of tele-education in healthcare. Hospitals using Polycom video for everything from clinical rounds to nursing training for students studying from their homes.
“Some hospitals, like Johns Hopkins, are using our mobile software, sending iPads home with patients after major surgeries and keeping them on track via video versus having them have come in for exam after exam after exam,” Knauf said. “They are just doing checkups and delivering better patient care.”
Knauf said that audio is the biggest differentiator for Polycom telemedicine technology.
“We have stereo audio, but we also have a mode called music mode, it’s a mode we’ve used in music education for a long time that gives a much more natural representation of a musical instrument,” he said. “We recently found hospitals using music mode to listen to heartbeats remotely because they have found that when you switch this music mode on you get amazing clarity. We made it to hear a guitar or piano more naturally. It’s the same with a heartbeat. It’s not being compressed like many video systems will do, which is unnatural.”
But Polycom also boasts about its video quality, where software and algorithms enable users to have high-quality video conversations from as low as 128kbps, Knauf said.
“In the case of tele-psychiatry, it is extremely important that a patient feels more than just comfortable, it has to be virtually equal to an in-person experience with a natural conversation both from an audio and video perspective,” he added.
Required hardware depends on the situation. For inpatient stroke care, for example, a video codec and a pan-tilt-zoom camera are required. But for other uses, only an Internet-connected device with a camera is required.
“For tele-psychiatry, the best method for the psychiatrist is to have our Real Presence Convene, a desktop video system with our high-powered codec in there, for the highest quality audio and video,” Knauf said. “That patient could be on an iPad or an iPhone or their PC.”
Polycom secures all of its data in flight and at rest with AES encryption, from its iPhone app to its computer software to its video codecs.
Polycom’s telemedicine systems do not directly interface with EHRs.
“It can’t just pull information from a database into our system,” Knauf said. “You can connect your computer to it or share from an iPad or other device to our video codec; you are just sharing content. You can pull up X-rays, MRIs, EKGs, but you are not pulling from the EHR database.”
Sherpaa Health
Sherpaa Health markets its telemedicine offering more as a service than a technology product.
“We don’t white label our technology,” said Jay Parkinson, MD, founder and CEO. “If we partner with a health system, they are purchasing Sherpaa as a service. We use our doctors. And the consumer behavior we want to change is before you go to a doctor in person, go online first, because 70 percent of things can be resolved online before you wind up in the emergency room or urgent care center.”
Sherpaa Health services come in many forms.
“We have a website and iOS and Android apps for patients, and the technology platform we built for our doctors facilitates their own practice, and their own practice is exclusively virtual, they never see you in person,” Parkinson said. “When members of Sherpaa create a case, if it’s a simple case, it takes 10 minutes, if it’s a complex case, it may take six months. We own that case from beginning to end. It’s not a sort of 10-minute video transaction. In many ways we’re a new type of delivery model rather than a technology.”
For example, a recent patient who signed up on Sherpaa Health in September 2016 ended up diagnosed with testicular cancer. Sherpaa arranged for all of his care and three days later he was home from surgery, the company said.
“We have a proprietary network of caregivers we can refer your care to if virtual diagnosis and treatment is not the right avenue you can take,” Parkinson said. “We either diagnose and treat you or diagnose and care coordinate you. The concept of having a CRM is a big deal. Most telehealth is if we can’t help you here, you are on your own again. But this is more of a hand-holding scenario throughout the situation.”
Ninety-eight percent of interactions between Sherpaa’s physicians and patients occur over asynchronous secure messaging; the remaining communications occur on the phone. In five years of operation, the company has used video communication twice, it said. Patients need only any device that can handle secure messaging via web browser or mobile app.
Sherpaa Health stresses that its technology and processes are HIPAA compliant and secure.
“No personal health information is part of the email notification you receive,” Parkinson said. “It just says you have a new message from Sherpaa. All the messages, labs and everything are contained within the secure app.”
However, Sherpaa Health’s telemedicine offering does not integrate with electronic health records.
“I do not believe that is the right move for us because we treat this more as a service,” Parkinson said. “The way we integrate is with digital faxes. Whenever we refer someone, the specialist gets a referral via fax, the specialist consult report we get back from the specialist is a digital fax, which is included in the case. Our problems are not billing and data problems, it’s communications issues to make sure our doctors and patients are working with the same information, and digital faxes connect everybody.”
SnapMD
SnapMD positions its virtual care management system as complete virtual point of care. It has a patient interface, a provider interface and an administrative back-end that enables health system staff to operate the platform and their telehealth program.
“It has communication tools like high definition video, multi-participant video, screen sharing for presenting medical images to patients remotely, diagnostic devices, a full file-sharing feature within the system, e-prescribing, a Dropbox-like feature, a full scheduling system that has the ability to manage all of your patients and their records, you can manage staff within the system, and run full analytics reports,” said George Tierney, chief operating officer and executive vice president of product development and marketing.
SnapMD said its system is akin to setting up a virtual clinic, with all the tools necessary to run a clinic.
“Anything you need to run and operate a medical practice, any telehealth program in a virtual environment,” Tierney said. “We have within the administrative interface a rules engine, it’s close to programming. You can create custom rules within the system. A rule might be please make sure the system double-checks that the patient verifies they are still within the state of their home address, or you can set rules that certain patients can only see certain providers based upon the state in which the provider is in.”
There also is a roles-based engine, where administrators can create roles and responsibilities that are quite broad or very narrow, then assign those roles to each staff member.
“We looked at everyone in the space, and we realized telemedicine is not a new carve-out service, that’s a mistake,” Tierney said. “By doing that, that is a massive limitation. Those in the market that are both developing the technology and delivering the service have a ceiling at which they can actually provide value. We decided we would build a system we would put in the hands of the existing healthcare providers and in order to do that we need to do that in a certain way.”
When SnapMD designed its system, it designed it on what is known as a self-consuming API construct, which supports data interoperability.
“We built the brains, the center of the system, and then built our front-end around it using those APIs, that we would then make available to our clients to do with as they want,” he said. “They want to do data integration with their systems, if they have plans to build complementary systems on top of our platform, they can do that.”
By using the API construct, it creates a self-regulating quality assurance because those APIs are not a side project, they are the center of attention and have to work at peak performance at all times, Tierney said.
“And because we are self-consuming our APIs, that means we can make our entire system available through APIs and SDKs,” he said.
The video and data connections are fully encrypted end to end. And the system does integrate with EHRs.
“This goes back to our APIs, the other system needs to be able to accommodate that integration,” Tierney said. “We are integrated with athenahealth, Allscripts, some custom with Epic and some of the others, and we also offer our clients an option to go with integration with Redox, which was founded three years old ago by members of Epic’s integration team. Redox is like a health information exchange, middleware, and they’ve integrated with the top 10-15 EHRs out there.”
Teladoc
Teladoc was founded 15 years ago, selling its telemedicine offering to large self-insured employers and then to health plans and over the last couple of years to hospitals and health systems.
“We did 952,000 visits in 2016, and will do more than 1.4 million in 2017, and a lot of scalability is required for that, and a lot of flexibility at the patient level so patients can use it in multiple modalities,” said Dan Trencher, senior vice president of product strategy. “We have Android and iOS mobile apps, a website, and a 24/7 call center that can support patients going through our registration process and into having a visit.”
“It’s intended to exchange, pulling from a health record or other type of clinical data repository as well as sharing data back out.”
The company performs quality assurance with a team of nurses that reviews patient charts to ensure patients are getting a quality experience, Trencher said.
“It’s not just a video connection between a doctor and a patient, it’s a service with high quality care baked in,” Trencher said. “And patient engagement is key. There is a high incentive to drive the behavior change so that consumer thinks of accessing telehealth when they have the need, or in other cases like in post-discharge cases when they want to check in. That further engagement, we have a bit of science around that, and we’re pretty good at it.”
Teladoc can be used where Teladoc physicians are teed up, where a health system’s doctors are the go-to clinicians, or where there is a combination of the two.
“We can wrap our physician network around theirs and set up business rules so that during the day during the week the consult request that comes in will first route to the doctors affiliated with the health system, but if they are not available then our network can wrap around that and provide care,” Trencher said. “Also, because the platform is built on a very open architecture and uses APIs as its core way of interacting, it’s built for connectivity and real-time data exchange, so we have real-time connectivity with 20-plus of our health payer partners as well as connectivity to exchange clinical data with care management platforms at a health plan through multiple different potential formats or channels.”
And the company takes security very seriously, Trencher said.
“We’ve been put through the wringer by having large clients who are financial institutions or health plans with tens of millions of members, we’ve had to answer long lists of questions in our RFPs. We have been tested in that way.”
And the Teladoc system integrates with EHRs.
Zipnosis
Zipnosis said health systems would implement its telemedicine offering for two reasons. The first is for downstream revenue from patients and access, and gaining a powerful way to drive the relationship with a patient, the company said. The second is the clinical efficiency in delivering very simple care, the company added.
“We have an independent study of one of our clients that showed about 25 percent of the new patients who used the system went on to develop an ongoing relationship with the health system that developed $3,000 of incremental revenue,” said Jon Pearce, CEO. “It’s about accessing and keeping those customers when they are making healthcare choices.”
Zipnosis provides four ways to interact with its telehealth platform. The first is through an asynchronous adaptive interview, something of a digital conveyer belt to get to the right care. The second is direct to video, the third is direct to phone, and the fourth is a triage tool, so a patient ultimately can schedule an in-clinic visit, if necessary. There is also a boarding pass mode that enables quick access to clinical tests.
“From our user research we know that younger, healthier patients do not want to do a video or phone visit, so offering them the asynchronous tools is the way to get them,” Pearce said. “We have the ability to take our tool set and match it to demonstrated patient preferences in the market and then tie that to an ROI.”
Patients and providers only need an Internet-connected device with a camera. They can access the system through a website or a mobile app.
“In the security realm, the system is cloud-based and we work with a third party that has a HITRUST certification,” Pearce said. “And PHI is only accessed after log-in, all the information is encrypted under SSL both in transit and in the database as well. It’s above industry standards.”
Zipnosis integrates its telemedicine system with various EHRs, including Epic, Cerner and athenahealth.
“Today we support HL7 and CCDA into those three EHRS,” Pearce said. “We also have single-sign-on so the platform can be embedded in an Epic or Athenahealth portal so the patient does not have to re-authenticate. And the whole application has an API wrapper for a customer that wants to truly embed the platform into their existing technology stack.”