(NEHI) 2004 report Remote Physiological Monitoring: Innovation in the Management of Heart Failure
New England Health Care Institute (NEHI) 2004 study advocates the cost saving value for heart failure patients to use remote patient monitoring (RPM). The facts showing a saving of $5,034 per patient per year when compared to standard care, regardless of some of the key barriers to the adaption of telehealth technology.
May 18, 2016
Study Published on July 1st 2004 by The New England Health Care Institute (NEHI)
Background
Remote physiological or patient monitoring (RPM) for heart failure, an innovative telehealth technology, was the subject of the New England Healthcare Institute’s (NEHI) 2004 report entitled “Remote Physiological Monitoring: Innovation in the Management of Heart Failure.” NEHI’s analysis of the available evidence demonstrated that using RPM for heart failure improves patient outcomes and decreases health care costs. Despite this potential, key barriers lie in the way of widespread adoption of RPM. The most significant barriers highlighted in the NEHI report include reimbursement shortfalls, clinician concerns and limited patient awareness of the technology.
NEHI has continued to work in this exciting area since publication of the 2004 report. In this update, we provide a cost-effectiveness analysis using the expanding evidence base for RPM, examine the status of barriers to adoption, and conclude with a look at coverage and reimbursement options.
Key Findings
- There is a 60 percent reduction in hospital readmissions compared to standard care and a 50 percent reduction in hospital readmissions compared to disease management programs without remote monitoring.
- Remote patient monitoring has the potential to prevent between 460,000 and 627,000 heart failure-related hospital readmissions each year.
- Based on this reduction in hospital readmissions, NEHI estimates an annual national cost savings of up to $6.4 billion dollars.
Update on the Value of RPM: Cost Effectiveness
Approximately 5.3 million people are living with congestive heart failure in the United States1 and 30 percent of these individuals2, 1.59 million patients, are Class III and Class IV heart failure patients. These patients represent the population that will benefit most from remote monitoring technologies. In order to estimate the national impact of the adoption of RPM technology, we compared RPM to both disease management and standard care in terms of the financial costs and reduction in heart-failure (HF) related readmissions associated with each care model. We used per patient per year estimates and then applied these estimates to the population of Class III and Class IV heart failure patients at large.
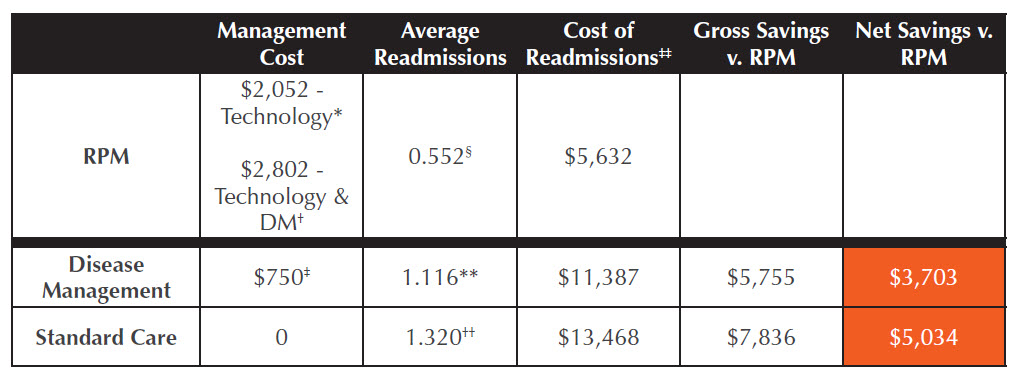
As shown in the table, “Heart Failure Care Comparison,” we estimated the average yearly cost of RPM to be $2,052 per patient for the technology alone and $2,802 per patient for the technology and the disease management program. Previous research has found that disease management programs cost an estimated $750 per patient per year and given that standard care does not include any disease management, there is no cost associated with that care model. Next, using the most recent available data, we found that patients using RPM technology have an estimated 0.552 HF-related readmissions per year (i.e. the likelihood of each patient being readmitted in one year is 55.2%) compared to 1.116 HF-related readmissions per year among patients receiving disease management without RPM and 1.320 HF-related readmissions per year among patients receiving standard care. Applying these readmission estimates to the cost of a HF-related hospitalization ($10,203 as reported by the Agency for Healthcare Research and Quality), we found that the yearly per patient cost of HF-related readmissions ranged from $5,632 for RPM patients to $11,387 for disease management without RPM patients to $13,468 for standard care patients. The gross savings of RPM technology as compared to disease management and standard care is $5,755 per patient per year and $7,836 per patient per year, respectively. The net savings (gross savings less incurred cost of intervention) are $3,703 per patient per year for RPM vs. disease management and $5,034 patient per year RPM vs. standard care.
Next, we applied these savings to all Class III and Class IV heart failure patients. Assuming that 80% of the 1.59 million patients in these two classes, or 1.27 million patients, will be hospitalized in a year, RPM can potentially yield a savings between $4.7 billion (if all eligible CHF patients are enrolled in disease management program and change to RPM) and $6.4 billion (if all eligible CHF patients are receiving standard care alone and change to RPM).
Heart Failure Care Comparison:
RPM vs. Standard Care and Disease Management, Per Patient Per Year
Barriers to Change
While the barriers to RPM adoption identified in NEHI’s 2004 report still remain, new information on these barriers is now available. Among the new developments are:
- Inadequate reimbursement: Medicare does not widely support remote health services, nor do about half of the state Medicaid programs, but approximately 130 insurance companies now provide coverage for telemedicine in some capacity.3,4
- Provider concerns: Providers remain concerned that telemedicine will generate large volumes of additional work, increase legal liability, and lead to the loss of traditional provider control.5
- Limited patient awareness: Patient awareness of RPM remains low because there is a limited amount of public information available and that which is available is not reaching the target audience – seniors, chronically ill and caretakers of the chronically ill or elderly.6
In addition to the barriers above, we identified three important information technology barriers to adoption of remote health services that were not included in the 2004 report 1) the lack of interoperable connectivity standards amongst providers to allow for the large scale adoption of RPM technologies; 2) spotty adoption of electronic medical records (a health information technology system that, many experts argue, should be a prerequisite for RPM adoption); and 3) the lack of infrastructure in rural areas. Even though remote technologies exist in the market today, the healthcare industry needs to resolve the barriers mentioned above to allow these technologies to diffuse widely in the marketplace.7
Coverage and Reimbursement Policy Options
In CMS’ 2009 final physician payment rule, new codes were created to report remote monitoring using RPM technology when the service meets a set of restrictive criteria. Although coverage for all RPM technologies and services remains uncertain, the new codes represent a key milestone toward broadened coverage prospects for these technologies. Potential strategies to obtain coverage for all RPM technologies are:
- Work with CMS Coverage with Evidence Development program allows Medicare to provide a provisional national coverage decision when there is insufficient evidence for unlimited coverage.8
- In the absence of national coverage, each of the CMS Regional Offices may pursue a Local Coverage Determination (LCD). In many circumstances, LCDs may improve the available evidence and demonstrate effectiveness. As is often the case with emerging technologies, a conglomerate of LCDs may lead to an NCD.9
As CMS and the Medicare Payment Advisory Commission look to redesign reimbursement system to encourage efficiency, a strong recommendation has been made to Congress to eliminate hospital payment for re-admission for the same condition within 30-days. To encourage hospitals to collaborate with post-acute providers to provide better care post-discharge, in conjunction with eliminating payment for re-admission, CMS should also provide incentive payments to hospitals that demonstrate a lower re-admission rate. Payment elimination will encourage the adoption of RPM and payment incentives will provide the financial support for those hospitals that incorporate RPM.
Conclusion
Since the publication of NEHI’s report on remote patient monitoring in 2004, there is growing evidence of the potential of RPM to reduce readmissions for heart failure patients. There is also new evidence of the technology’s cost effectiveness. Despite these potential benefits of RPM, barriers to its adoption remain and the coverage and reimbursement options are still limited. NEHI continues to work with Dr. Steve Phurrough, the Director of the Coverage and Analysis Group at CMS, to determine what evidence NEHI could provide to speed CMS’s RPM coverage decision.
Text Endnotes
1.Heart Disease and Stroke Statistics – 2008 Update. American Heart Association and American Stroke Association, 2008.
2.University of Califorina at San Francisco Medical Center. Heart Failure – Diagnosis. http://www.ucsfhealth.org/adult/medical_services/heart_care/heart_fail- ure/conditions/failure/. Accessed November 4, 2008.
3.AMD Telemedicine. Private Payer Reimbursement Directory. http://www.amdtelemedicine.com/private_payer/index.cfm. Accessed on May 29, 2008. 4Haselkorn A, Coy MJ, Doarn CR. The future of remote health services: summary of an expert panel discussion. Telemedicine and e-Health, 2007; 13(3):341- 347.
5.Health Technology Center. The future of remote health services: technology forecast report. San Francisco: HealthTech; 2006
6.Boehm EW, Manning H and Geller S. Healthcare Unbound’s Awareness Challenge: How to Make Consumers Want the Remote Monitoring Solutions They
Need. Cambridge: Forrester Research, Inc.; 2007.
7.Health Technology Center. The future of remote health services: technology forecast report. San Francisco: HealthTech; 2006.
8.Centers for Medicare and Medicaid Services. National coverage determinations with data collection as a condition of coverage: Coverage with Evidence
Development. Baltimore: CMS; 2006. http://www.cms.hhs.gov/mcd/ncpc_view_document.asp?id=8. Accessed on May 21, 2008.
9.Expert interviews.
Table Endnotes
* Average technology cost estimate was derived from data published in studies cited below and through expert interviews with technology companies.
† Average monthly technology cost estimate of $171 results in $2,052 yearly cost. Including the average disease management cost per year of $750 results in a $2,802 yearly cost for both RPM technology and the disease management component.
‡ Average disease management cost based on the $750 base case estimate cited in Chan et al. and re-calculated for a per month estimate.
- Average hospital re-admission rate based on 2 published studies (Benatar et al., Weintraub et al.) and unpublished data from a study at the Center for Con- nected Health.
** Ibid.
†† Average hospital re-admission rate based on study published by Knox et al.
‡‡ Average cost of a congestive heart failure-related hospitalization was $10,203 in 2006 according to the HCUP database.
Studies Used in Cost Comparison Calculations
Benatar D, Bondmass M, Ghitelman J, and B Avitall. Outcomes of chronic heart failure. Archives of Internal Medicine, 2003;163(3):347-52.
Chan D, Heidenreich P, Weinstein M, and G Fonarow. Heart failure disease management programs: A cost-effectiveness analysis. American Heart Journal,
2008; 155(2): 332-338.
Knox D, et al. Implementing a congestive heart failure disease management program to decrease length of stay and cost. Journal of Cardiovascular Nursing, 1999; 138(4): 633-40.
Weintraub AR, C Kimmelstiel, D Levine, et al. A multicenter randomized controlled comparison of telephonic disease management vs. automated home
monitoring in patients recently hospitalization with heart failure: Span CHF II Trial. Journal of Cardiac Failure, 2005;11(9):720.