The economics of a comprehensive care management program in 2022
Care management services are reimbursable remote medical services that provide ongoing care to patients between traditional or remote doctor’s office visits. Such services include chronic care management (CCM), remote patient monitoring (RPM), behavioral health integration (BHI), and many others, with even more services emerging regularly.
Since their inception, care management services have largely been conceptualized as a series of discrete services that are implemented separately from each other and other telehealth services. Since the COVID-19 public health emergency began, Medicare and other payers have permanently widened the scope and increased the reimbursement of care management programs, supporting the creation of multi-service wellness programs that improve patient outcomes and engagement. These developments have also provided fee-for-service healthcare organizations with a strong, recurring source of revenue and risk-sharing organizations with substantial savings.
This column will largely focus on the economics of creating and implementing a comprehensive care management program. But before diving into this subject, I thought it may be helpful to provide some clarification regarding common misunderstandings surrounding care management programs, telehealth, and telemedicine.
We begin with a note about telehealth: Telehealth as a term encompasses the full spectrum of remote healthcare, including virtual visits, care management services, health applications, and connected medical devices. The ability to manage patients outside of the confines of an office has always promised to change the course and accessibility of modern medicine, and the pandemic has prompted much faster adoption than anyone could have anticipated.
Care management services are an important aspect of telehealth, yet the services are often thought as discrete, as noted above. It is becoming clearer that such conceptualization does a disservice to patients and providers. For patients, this interpretation is causing confusion about the value of care management services, why they are worth enrolling in and, when required, why they are worth paying co-insurance for. For many providers, the increasing number of care management service types creates uncertainty around value and investment, and how to fit care management into their organization’s workflow and goals.
As will be discussed, there is substantial value to providers and patients in implementing care management services as a more fluid set of tools in an overall comprehensive patient care program — essentially an à la carte menu that can be tailored to provide patients with care management they need in timelier and more efficient manner. Such a program is not just beneficial for patients. With the recent coverage and reimbursement changes, a comprehensive care management program can also make a significant difference in a healthcare organization’s bottom line.
Changed landscape of care management
The issuing of the 2022 Physician Fee Schedule (PFS) final rule made it even more apparent that organizations seeking to expand or implement patient care management programs will be best served by taking a comprehensive approach — one that allows patients to receive a wider range of services tailored to their individual needs while better ensuring reimbursement for all aspects of those services.
These terms all speak to a program that combines the offering of CCM and RPM services, which are sometimes supplemented by additional care management and preventive services. Regardless of how you describe the program, developing such a program can deliver significant benefits to patients and providers. For patients, a comprehensive care management program will help them receive more timely, personalized, preventive care that contributes to overall better health and improved access to care. This naturally translates to fewer hospitalizations and readmissions as well as lower costs for patients and the healthcare system.
That alone makes offering comprehensive care management to your patients worthwhile. But the thick icing on the cake is that by combining CCM, RPM, and, when appropriate, other patient-specific care management services, the bottom line of organizations will benefit from a consistent, high-revenue-generating service. That’s the focus of this column.
To help you gain a better understanding of the economics behind a comprehensive care management program, we’re going to take a high-level look at the three most common patient cohorts that would be covered under such a program. We’ll discuss how CCM and RPM services would apply to these cohorts and how these services are currently covered and reimbursed by Medicare.
Patient cohort #1: Two or more chronic conditions + RPM device
This first patient cohort is likely to reflect the most common comprehensive care management service opportunity: a patient with two or more chronic conditions receiving CCM services whose health and wellness is further supported by an RPM device.
Consider that data show nearly 70% of Medicare beneficiaries have two or more chronic conditions, with the most common including hypertension, obesity, congestive heart failure, chronic obstructive pulmonary disease, and diabetes. These beneficiaries would be eligible for CCM services.* This includes the development of a comprehensive, patient-specific care plan with goals and then ongoing, monthly support to help patients achieve those goals and reduce the need for additional healthcare services.
If one of the chronic conditions can be supported by an RPM device, such as a blood pressure monitor, weight scale, blood glucose meter, or pulse oximeter, organizations can provide patients with a device and bill for furnishing RPM services. This includes providing the device to beneficiaries and educating them on its use, and then the ongoing capture and review of device-transmitted data.
Now that we’ve established a general understanding of CCM and RPM, let’s look at a common patient scenario for this cohort and what organizations would bill for supporting such a patient. Mr. Jones has been diagnosed with hypertension and diabetes. He is enrolled by his provider in a comprehensive care management program and provided a blood pressure monitor that captures and transmits systolic, diastolic, and heart rate readings to his provider. Mr. Jones receives monthly CCM and RPM services delivered by the provider’sclinical staff for the next 12 months. Here’s what the provider could bill for the services:
- For the CCM services, about $62 per month for up to 20 minutes of services. (Note: Each additional 20 minutes in a given month, up to two times, is billable at about $47 each, but most patients will not require services more than 20 minutes).
- For the RPM device services, the provider would bill about $18.50 for the service initiation. It would then bill about $54 for the monitoring and management of the monthly data transmission.
Over 12 months, assuming CCM services do not exceed 20 minutes in any given month, the organization would receive $1,410.50 in Medicare reimbursement for delivering comprehensive care management services to this individual patient — $744 in CCM-related services and $666.50 in RPM-related services.
*Depending upon the severity of a patient’s chronic conditions, they may be eligible for complex CCM, which requires more extensive services but is also reimbursed higher. Since most patients will not require complex CCM, we’re going to focus our discussion on non-complex CCM.
Patient cohort #2: Two or more chronic conditions, no RPM device
For this second cohort, we look at patients with two or more chronic conditions who cannot use or are not provided an RPM device. Considering the rapid growth in the availability of RPM devices to support various chronic conditions, most patients will be able to benefit from an RPM device. But there are scenarios where a patient does not have a chronic condition that can be supported by a device or the provider is unable to provide one — either by choice or if the patient has already been provided an RPM device by another provider.
Consider Mrs. Smith, who has osteoporosis and arthritis. She is enrolled in a comprehensive care management program to receive support for these conditions. Over 12 months, assuming CCM services do not exceed the initial 20-minute reimbursement threshold in any given month, the organization could bill Medicare the same $744 as was billable for the CCM-related services discussed in patient cohort #1.
Patient cohort #3: One chronic condition + RPM device
Statistics indicate that close to 90% of Medicare beneficiaries report at least one chronic illness. If we assume that 70% have two chronic conditions, that leaves us with about 20% with a single condition. These patients would not be eligible for CCM. In such a situation, the patient is likely to “default” to care management via RPM.
A patient enrolled in full RPM services has a chronic condition that’s less severe and/or requires less direct management than dictated by the structure of CCM regulations. As such, RPM services at this time do not require the creation of an individualized care plan for enrollees but still reimburse care teams for time spent managing these patients.
Such patients who would only receive RPM services are those with acute conditions and then post-acute procedure support. Common examples:
- Patient is taking part in a medical weight loss program
- Patient has COVID-19 and receives a pulse oximeter to report back for the duration of the disease
- Patient gets an ablation for heart rhythm issues, then receives an ECG monitor post-discharge for one month of monitoring
- Patient is pregnant and receives a blood pressure monitor to watch for gestational hypertension
The reimbursement math on this scenario is straightforward: Mr. Williams is obese and receives a weight scale as a part of his weight loss program. The provider would bill about $18.50 for the service initiation and then could receive $54 for each month of monitoring and management of the monthly data transmission.
What is important to note about this cohort is that although the 2022 fee schedule lowered the RPM device-supply reimbursement, a well-run RPM program can still prove profitable in 2022. The decision by CMS to decrease RPM reimbursement can be inferred as the agency further encouraging organizations to bring RPM under a broader comprehensive care management program.
Comprehensive care management program by the numbers
We’ve thrown a lot of information and numbers at you, so we thought it would be helpful to represent what we’ve covered in a chart. The following identifies the cohorts we’ve discussed, estimated reimbursement for enrollment and monthly services (these will vary with geography and other factors), key requirements to know for each cohort, and the CPT codes you may use for billing each of the cohorts
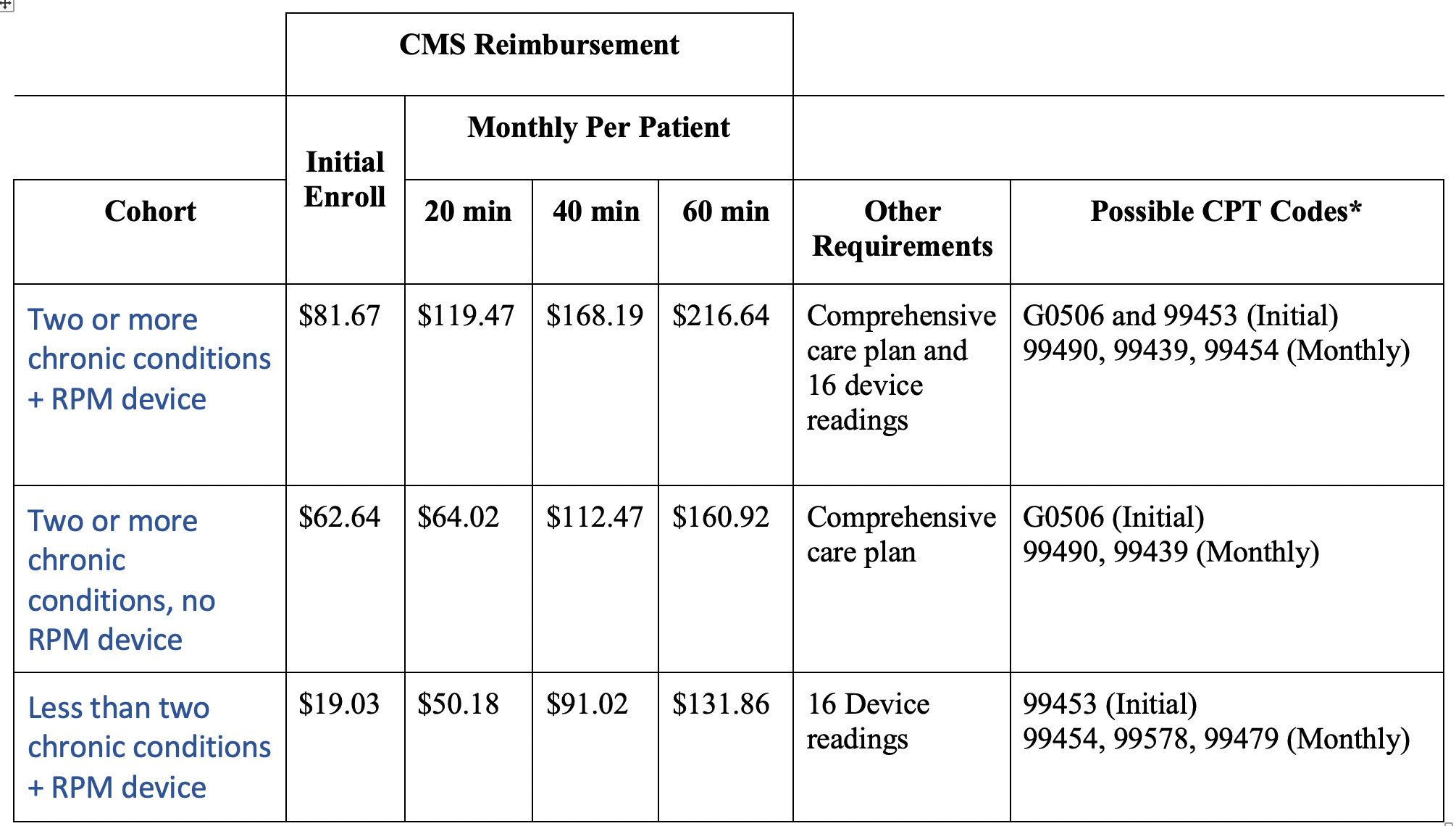
* Each CPT code has its own set of documentation requirements. Always consult a medical billing professional to make sure you are following all requirements.
Looking at the above chart, let’s consider a cardiologist with a patient population of 400 medium- and high-risk patients. Of those, assume 200 have hypertension and hyperlipidemia and are provided a blood pressure cuff; 150 have just heart failure and are given a weight scale; and the remaining 50 have two chronic conditions but don’t require an RPM device.
Assuming these 400 patients are enrolled in a care management program and the minimum amount of time is allocated for each patient interaction (20 minutes), here’s a breakdown of the monthly fee-for-service revenue the cardiologist can expect to generate:
- For the 200 patients with hypertension, hyperlipidemia, and a blood pressure cuff: ~$24,000 per month (200 x $119.47)
- For the 150 patients with heart failure and a weight scale: ~$7,500 per month (150 x $50.18)
- For the 50 patients with two chronic conditions and no device: ~$3,200 per month (50 x $64.02)
Over a 12-month period, these patients will generate more than $416,000 in revenue for the cardiologist. This does not include the one-time enrollment fee for each of the 400 patients, which would generate an additional $22,000 in revenue.
Taking care management to an even higher level
CCM and RPM are just a few of the components that organizations should incorporate into their comprehensive care management programs. The strongest programs will use a mix of the care management services best suited to meet patients’ specific conditions and risks, with those services evolving to reflect any changes in a patient’s conditions and/or health and wellness goals. When care management services are incorporated into a program and delivered effectively, providing organizations and their patients reap significant clinical and financial benefits.

