What remote patient monitoring means for heart failure
Remote patient monitoring positive outcomes far exceed conventional care for heart failure patients!
February 10, 2016 by Jodi Askew
Now more than ever, cardiovascular service line leaders are expressing interest in deploying telemonitoring technology to remotely manage their CV patients. Remote patient monitoring, or RPM, enables providers to virtually collect and transmit a patient’s data for the purposes of clinical assessment and care management. The health care IT community is largely in agreement about RPM’s potential to expand the geographic reach, clinical scope, and capacity for quality care—isn’t it about time our CV service line leaders joined the conversation?
We say “yes.” Just last year, our Health Care IT Advisor research team suggested that providers should deploy RPM for chronic disease patients. This has become more important in the last year, with mounting pressure from CMS and private payers to expand the timeframe for long-term accountable care management in the CV service line and escalating penalties associated with excess readmissions.
With this in mind, we examined the recent literature on the clinical and financial impacts of RPM for heart failure (HF) patients in five high-impact areas—length of stay, mortality, readmissions, cost effectiveness, and reimbursement—and have reported our most interesting findings below.
Length of stay
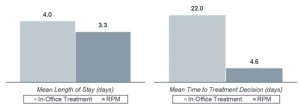
A recent Health Information Management System Society (HIMSS) study found RPM delivered impressive results when compared to in-office treatment by reducing the time required for clinicians to make treatment decisions and cutting length of stay largely as a result of reduced health care utilization during the patient’s CV hospitalization, as well as during any additional clinical events requiring hospitalization in follow-up.
Mortality
With an ever-growing focus on quality metrics, hospitals are increasingly accountable for patient outcomes—and now, there’s significant evidence that RPM can improve one key measure: mortality. A 2015 meta-analysis of thirty randomized control trials on use of RPM among HF patients found that telemonitoring reduced the risk of mortality by 53% when compared to conventional care. A Cochrane Library Literature Review of 25 peer review studies on the subject reached similar findings, concluding that telemonitoring reduced the risk of all-cause mortality in patients with congestive heart failure (CHF) by 34% compared to conventional care.
Readmissions
RPM can also be an effective tool in the CV leader’s arsenal to avoid the substantial penalties introduced by the readmissions reduction program. Since its start in 2008, Geisinger Health Plan’s telemonitoring program reduced the risk of all-cause readmission for their Medicare Advantage plan members by 77%, and reduced the risk for 30-day and 90-day readmission by 56% and 62%, respectively. The 2015 meta-analysis of thirty randomized trials further underscored the power of RPM to reduce readmissions, finding that telemonitoring was associated with a 64% reduced risk for readmission related to HF.
Cost effectiveness
We expect that by now you’re now wondering—what about the money? Well, the ROI on Geisinger Health Plan’s telemonitoring program was 3.3. Furthermore, a New England Health Care Institute study suggested that RPM for cardiac patients would result in a net savings of $5,034 per patient per year when compared to standard care.
Reimbursement
Telehealth (in the form of live, interactive audio-visual communication) has gained greater reimbursement coverage in recent years, and RPM seems to be following suit. In fact, Peter Kilbridge, a senior researcher at the Advisory Board and telemedicine expert, recently told The Daily Briefing that he anticipates the vast majority of telemedicine services will become reimbursable.
However, RPM differs from the traditional forms of live, audio-visual telehealth, in that it is characterized by store-and-forward asynchronous (not-real-time) data transmission with a health care provider. Coverage for RPM, as opposed to telehealth, is largely based on this store-and-forward distinction. While the coverage determination for RPM is decided state-by-state, CMS is encouraging ACO participants in particular to take advantage of the shared cost associated with RPM as per the guidelines of the Medicare Shared Savings Program (MSSP), with the overall goal to enhance care coordination.
At the start of this year, New York joined several other states in expanding telehealth reimbursement parity legislation to require commercial insurers as well as the state’s Medicaid program to provide reimbursement for RPM. At this time, fifteen states reimburse RPM activities to varying degrees. To learn about RPM coverage in your state, look to the American Telemedicine Association’s State Policy Resource Center, which provides a regularly-updated overview of policy considerations in each of the 50 states.