
Medicaid


Congress reaches major health policy deal on Medicare, Medicaid, and pandemic preparedness
WASHINGTON — Leaders in Congress have reached a sweeping deal to ease Medicare pay cuts to doctors, make major changes to post-pandemic Medicaid policy, and to help prepare for future pandemics. Lawmakers are aiming to pass a health care policy package along with legislation to fund the federal government by Friday. The details of the omnibus […]

Biden administration extends COVID-19 public health emergency
WASHINGTON (AP) — The Biden administration said Thursday that the COVID-19 public health emergency will continue through Jan. 11 as officials brace for a spike in cases this winter. The decision comes as the pandemic has faded from the forefront of many people’s minds. Daily deaths and infections are dropping and people — many of them maskless — are returning […]

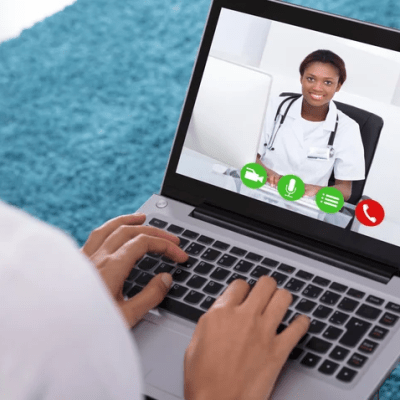
Emerging State Policies, CMS Telehealth Policy Updates & Hope for PHE Policy Extension
As the Center for Connected Health Policy has continued to update our Telehealth Policy Finder over the course of 2022, a few new elements are beginning to emerge in newly passed legislation and in adopted Medicaid policies. While these may not yet be trends, they have potential to develop into trends, as it is common […]


Public Health Emergency Set for Extension: Lack of Notice Implies Renewal through Mid-October
The declared Public Health Emergency (PHE) under the Public Health Service Act will apparently be renewed at least one further time beyond its current July 15, 2022 expiration, as the Department of Health and Human Services (HHS) has repeatedly committed to provide a 60-day notice prior to the termination or expiration of the PHE, and mid-May has […]

Fact Sheet: Biden-Harris Administration Announces Additional Actions in Response to Vice President Harris’s Call to Action on Maternal Health
APRIL 13, 2022•STATEMENTS AND RELEASES Vice President Harris to Host First-Ever Meeting with Cabinet Officials on Maternal Health On Wednesday, April 13, 2022, during Black Maternal Health Week, Vice President Kamala Harris will convene a meeting with Cabinet Secretaries and agency leaders to discuss the Administration’s whole-of-government approach to addressing maternal mortality and morbidity. The […]
Bipartisan Bill Aims to Increase Access to Virtual Mental Health Services
Three US senators have introduced legislation to increase access to virtual mental health services for children and underserved populations. By Mark Melchionna April 12, 2022 – To expand access to virtual mental health services, US Sens. Sherrod Brown (D-OH), John Thune (R-SD), and Ben Cardin (D-MD) have introduced the Medicaid Ensuring Necessary Telehealth is Available Long-term (MENTAL) Health for […]
HHS extends COVID-19 public health emergency for another 90 days
By Robert King Apr 13, 2022 03:11pm The Department of Health and Human Services (HHS) has extended the COVID-19 public health emergency for another 90 days and potentially for the final time. The PHE, which gives key flexibilities to providers and states, will not expire in July. The PHE was originally expected to expire April 16. It […]

4 Remote Patient Monitoring Reimbursement Tips for Your Practice
By: Collin Couey on March 25, 2022 Imagine spending precious time and money setting up a remote patient monitoring program at your practice only to realize it’s too costly to maintain. If you’re on the fence about setting up such a program, you can avoid that worst-case scenario. We’ll break down the ins and outs of remote patient monitoring […]

Congress Considers Extending Medicare Telehealth Flexibilities
During the COVID-19 pandemic, HHS has allowed numerous telehealth flexibilities across Medicare and Medicaid, making it possible for patients to receive care remotely from their homes and enabling states, managed care organizations, and providers to expand access to care. The telehealth landscape looks drastically different now compared with before the pandemic, with patients and providers […]
Mississippi Medicaid Reimbursement – Telehealth
Mississippi Last updated 01/13/2022 POLICY Policy applies to Private payers, MS Medicaid and employee benefit plans “Remote patient monitoring services” means the delivery of home health services using telecommunications technology to enhance the delivery of home health care, including: Monitoring of clinical patient data such as weight, blood pressure, pulse, pulse oximetry and other condition-specific […]

Mississippi Medicaid – MS Admin. Code 23 Part 225 Chapter 1 – Telehealth Services
Title 23: Division of MedicaidPart 225: TelemedicineChapter 1: Telehealth ServicesRule 1.1: DefinitionsThe Division of Medicaid defines telemedicine as a method which uses electronic informationand communication equipment to supply and support health care when remoteness disconnectspatients and links primary care physicians, specialists, providers, and beneficiaries whichincludes, but is not limited to, telehealth services, remote patient monitoring […]
HHS renews COVID-19 public health emergency order for another 90 days
By Robert King Jan 14, 2022 11:27am Department of Health and Human Services Secretary Xavier Becerra has renewed the COVID-19 public health emergency for another 90 days, extending key flexibilities for providers still grappling with the pandemic. The public health emergency was first ordered back in January 2020 and was set to expire after Jan. 16. […]

Outlook for the 2022 Federal Health Legislative Landscape
As the 117th Congress moves into its second legislative session, there is no shortage of health care policy issues dotting the landscape. The COVID-19 pandemic, legislative gridlock and a 2021 that was largely locked down by ongoing negotiations around the infrastructure and Build Back Better packages have left a range of stakeholders looking and hoping […]
