Coronavirus Daily Update: Skilled Nursing Occupancy Slips; US Begins Withdrawal from WHO
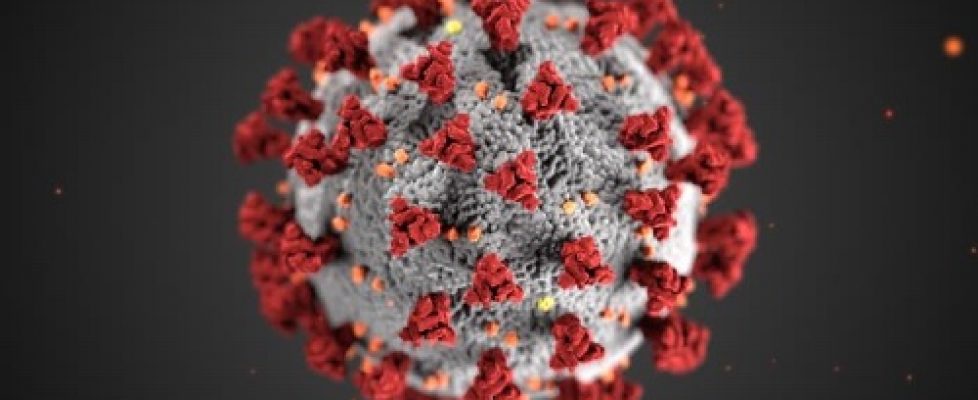
During this critical time, Home Health Care News remains committed to bringing you all the essential news related to home-based care operations. At the same time, we also recognize the seriousness of the COVID-19 pandemic. In addition to our regular content, we’ll continue to highlight industry-related developments and mitigation strategies in this rolling bulletin.
What you need to know from Wednesday (July 8):
— The Trump administration has officially notified the United Nations of its withdrawal from the World Health Organization (WHO), although the pullout won’t take effect until next year, according to the Associated Press.
— Overall, Congress has appropriated $2.6 trillion in funding to help the nation recover from COVID-19 and its impact on the U.S. economy. A new report from the Government Accountability Office (GAO) analyzed how the funding has been distributed thus far. As of May 31, the government has distributed $1.2 trillion in relief to individuals, businesses, health care providers and governments agencies. Only a fraction of that amount has gone to home health and home care agencies.
— Occupancy at U.S. skilled nursing facilities (SNFs) slid to 78.9% during the first peak of the COVID-19 pandemic in April, according to recent data from the National Investment Center for Seniors Housing & Care (NIC). That figure compares to 84.4% occupancy in April 2019. The occupancy dip may continue for the foreseeable future, especially as home health care providers ramp up their SNF-to-home diversion efforts.
— An estimated 5.8 million Americans 65 and older are living with Alzheimer’s dementia in 2020. By 2050, that number is projected to grow to upwards of 13.8 million people. As COVID-19 spreads across the globe, Alzheimer’s research is being delayed or suspended, with some of the most promising studies being forced to a complete halt, according to the American Neurological Association.
— As coronavirus cases surge, hospitals, nursing homes and other health care providers continue to face a dire shortage of respirator masks, isolation gowns and disposable gloves, reports The New York Times.
What you need to know from Tuesday (July 7):
— Small businesses have another month to apply for loans under the Paycheck Protection Program (PPP). President Donald Trump extended the program deadline to August 8 over the weekend. There is still about $130 billion left in PPP funding available.
— The Small Business Administration (SBA) and the Treasury Department released a list of more than 650,000 PPP loan recipients on Monday. However, the list was not exhaustive: It only included companies that received more than $150,000, accounting for less than 15% of all loan recipients. Among those included were Kanye West’s clothing and sneaker brand Yeezy, Ice Cube’s professional basketball league and a number of large fast food franchisees.
— While the SBA didn’t name all 5 million companies and organizations that have received PPP loans thus far, it did break down loan recipients by the numbers. Turns out, health care and social services businesses have been the top recipients so far, accounting for about 12.9% of the $591 billion in loans paid out.
— April — when the coronavirus was at its peak — was a banner month for telehealth usage. Telehealth claim lines increase 8,336% nationally from April 2019 to April 2020, according to FAIR Health’s Monthly Telehealth Regional Tracker. A claim line is an individual service listed on an insurance claim. The increase came after telehealth claim lines increased 4,347% from March 2019 to March 2020.
— Nursing homes workers were largely to blame for widespread facility outbreaks in New York, the state health department claimed in a report released Monday. The health department claimed facility staff — rather than residents — played the biggest role in spreading the virus throughout nursing homes.
What you need to know from Monday (July 6):
— The Trump Administration and CMS are taking additional steps to support access to home dialysis treatment, including newly proposed changes to the Medicare End-Stage Renal Disease (ESRD) Prospective Payment System (PPS). The proposed changes build on President Donlad Trump’s previous Advancing American Kidney Health executive order. Specifically, CMS is proposing that certain new and innovative equipment and supplies used for dialysis treatment of patients with ESRD in the home would qualify for an additional Medicare payment. Currently, more than 85% of Medicare fee-for-service beneficiaries with ESRD travel to a facility to receive their dialysis at least three times per week.
— Lawmakers in Colorado have approved a bill that will permanently expand telehealth coverage and access in the state, according to mHealthIntelligence. The bill requires the state Medicaid program to pay for telehealth services at rural health clinics, federally qualified health centers and the federal Indian Health Service at the same rate as in-person treatment. The bill also expands coverage to include home health and hospice care, among other services. The bill additionally allows home health care providers to supervise their own telehealth services.