mTelehealth™ Virtual Exam, Remote Health, Patient, and Therapeutic Monitoring Solutions
A complete solution to virtually and remotely collect, store, and report accurate health information for the best in patient-centered care.
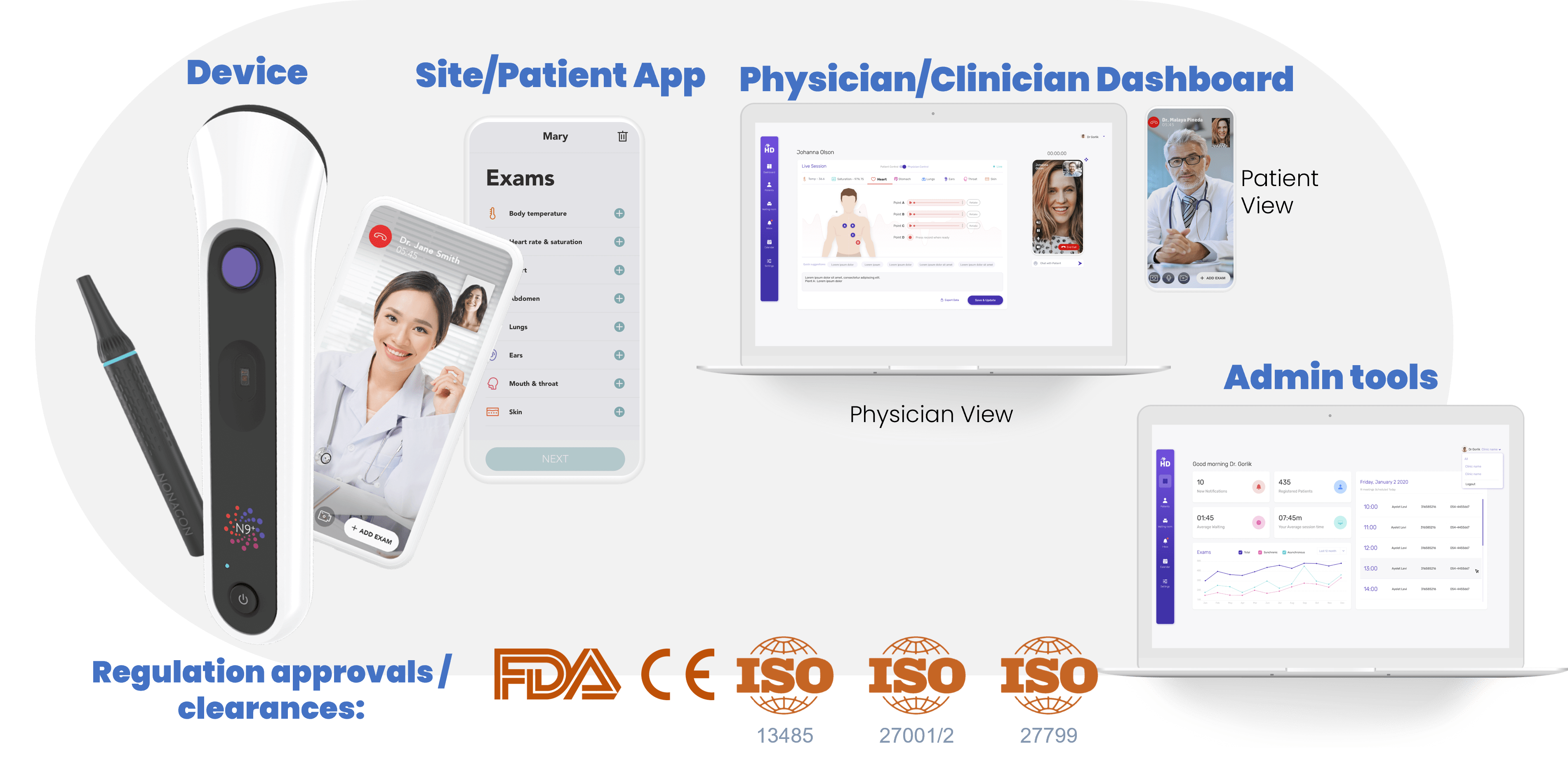
Introducing the Revolutionary Nonagon N9+ Virtual Telehealth Exam Device and Platform
The Future of Health Is In Your Hands